Three-dimensional breast imaging methods such as breast CT overcome the shortcomings of 2D mammography, in which overlapping structures can obscure cancerous lesions. Performing breast CT with synchrotron radiation (SR-BCT) enables the use of phase-contrast techniques, which produce images with high soft-tissue contrast. Now, researchers in Italy are planning the first clinical study of phase-contrast SR-BCT.
"In conventional attenuation-based x-ray imaging, the radiographic contrast comes from differences in volume density and composition between tissues. Attenuation-based mammography is limited by the intrinsically low contrast between glandular (healthy) and tumor tissue," explained Giovanni Mettivier, PhD, from the University of Naples "Federico II" and the Istituto Nazionale Di Fisica Nucleare. "On the other hand, in phase-contrast imaging, the image contrast comes from comparatively higher differences in electron density of tissues, giving the possibility of increased sensitivity through an increased image contrast of mass lesions."
The pilot study will take place at the Elettra synchrotron facility, which has been already used to perform phase-contrast mammography on more than 80 patients. The new study, called SYRMA-CT, will extend this clinical program to breast tomography, using phase-contrast CT with a single-photon counting detector. "In the SYRMA-CT collaboration, we plan to scan the first patient for breast CT in 2017," Mettivier said. "After successful completion of this project, a clinical trial is envisaged."
 Members of the dosimetry group of the SYRMA-CT project (from left to right): Christian Fedon, Antonio Sarno, Francesca Di Lillo, and Giovanni Mettivier.
Members of the dosimetry group of the SYRMA-CT project (from left to right): Christian Fedon, Antonio Sarno, Francesca Di Lillo, and Giovanni Mettivier.Dose considerations
To perform in-vivo SR-BCT of an entire uncompressed breast, the limited height of the x-ray beam (typically a few millimeters) necessitates translation and rotation of the patient. To minimize exam duration, the SYRMA-CT team plan to only image a 30 mm-high section of the breast, in regions where a suspicious lesion has been previously located. This strategy, however, has important dosimetric consequences.
The dose delivered in breast imaging is assessed using the mean glandular dose (MGD) to total mass of the breast. When only part of the breast is irradiated, however, MGD can underestimate this dose. Mettivier and colleagues designed a Geant4 Monte Carlo (MC) code to evaluate dose in such cases, introducing two new parameters: MGDv and MGDt. MGDv is the ratio between the energy deposited in and the glandular mass of the irradiated volume; MGDt is the ratio between energy deposited in the glandular mass of the whole breast and the glandular mass of the irradiated volume (Physics in Medicine and Biology, 18 December 2015, Vol. 61:2, pp. 569-587).
To validate their MC code, the researchers used it to simulate a conventional mammography exam with acquisition conditions reported in a previous study (Med. Phys. 19 April 2002, Vol. 29, pp. 869). For 5-cm thick compressed breasts with glandular fractions of 0%, 50%, and 100%, excellent agreement was seen between the simulated normalized dose coefficients in the two studies.
They also compared MC-simulated dose values with those reported in the literature for two breast CT studies (Med. Phys.Vol. 31, pp. 226) and Phys. Med. Biol. Vol. 59, pp. 2199). The maximum deviations between simulated and published data were 3% above 18 keV, and 3% over the whole energy range, for the two papers respectively.
Partial irradiation
To investigate differences in calculated dose for a whole and a partially irradiated breast, the researchers used their MC code to simulate a SR-BCT setup. They evaluated the dose delivered to a 12-cm diameter breast with glandular fractions of 0%, 50%, and 100%, for whole-breast irradiation, single-slice acquisition, and partial-breast irradiation.
For whole-breast irradiation, they calculated MGD as a function of photon energy (8 keV to 50 keV) for beam heights of 3 mm (translated to irradiate the whole breast) and 90 mm. Results showed that MGD decreased with increasing glandular fraction, and was not dependent on beam height.
For partial-breast irradiation, the beam height was fixed at 3 mm and the height of the irradiated volume varied from 3 cm (single-slice irradiation) to 87 mm, by translating the beam in 3 mm steps. This setup is close to the scan conditions that will be used in the SYRMA-CT project.
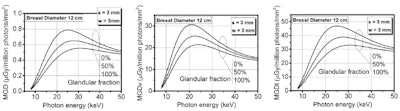
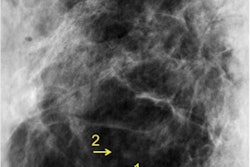
Left: MGD calculated on the entire breast mass as a function of photon energy, when only a slice of 3 mm of height is irradiated. MGDv (center) and MGDt (right) evaluated in the single 3-mm irradiated slice. Data are represented as lines for ease of visualization.
Plotting MGV, MGDv and MGDt as a function of photon energy for irradiation of a 3 mm slice revealed that MGDv and MGDt were significantly higher (up to 97%) than MGD. This finding confirms that the use of MGD when irradiating part of the breast underestimates the delivered dose, with the amount of underestimation increasing as the irradiated volume is reduced.
The researchers also examined MGD, MGDv, and MGDt for a glandular fraction of 50%, at 38 keV (one of the energies to be employed in the SYRMA-CT project), as a function of the height of the irradiated volume. MGD showed a linear dependence on height, while MGDv increased sublinearly. MGDt was almost independent of the height of the irradiated volume, and assumed values similar to MGD for the whole-breast irradiation.
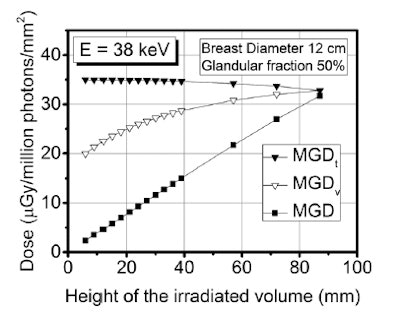 MGD, MGDv, and MGDt for a 12-cm diameter breast phantom with a glandular fraction of 50%, at 38 keV, varying the dimension of the irradiated volume with a 3-mm-height beam.
MGD, MGDv, and MGDt for a 12-cm diameter breast phantom with a glandular fraction of 50%, at 38 keV, varying the dimension of the irradiated volume with a 3-mm-height beam.The authors propose that in breast imaging exams where only partial irradiation is planned, MGDt is the most suitable metric for expressing the glandular dose to the breast. For SYRMA-CT, they plan to use their MC code to estimate the dose to glandular breast tissue prior to each x-ray exam. "It will be the basis of the dosimetric protocol for pilot breast CT scans at the Elettra synchrotron radiation facility, to be submitted to the regulatory board for study approval," Mettivier told medicalphysicsweb.
In future work, the MC code will be used to optimize patient acquisition protocols via a trade-off between image quality and glandular dose. Ongoing code upgrades will also enable estimation of the 3D distribution of glandular dose in the irradiated breast. "A final stage of the code development, to be implemented during the next year, will include a calculation of a patient-specific dose estimate after the exam, by including a description of the breast anatomy as provided by the CT scan," Mettivier said.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.