Shear-wave elastography performs better than B-mode and power Doppler ultrasound for evaluating tendinopathy and helping to assess treatment response, German researchers recently reported at the RSNA 2015 meeting in Chicago.
Not only was shear-wave elastography more sensitive for detecting tendinopathy in a prospective study, but the technique's quantitative data had much higher correlation with clinical examination scores, according to presenter Dr. Timm Dirrichs of University Hospital RWTH Aachen in Aachen, Germany.
"Shear-wave elastography provides an objective, quantitative assessment of tendon integrity and might be useful to guide treatment and develop new treatment approaches," Dirrichs said.
Common diseases
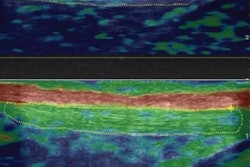
Insertion tendinopathies of the Achilles and patellar tendons are common orthopedic diseases, especially among young athletes. While sonographic imaging has traditionally been used in these patients to assess morphologic changes via B-mode and perfusion changes via power Doppler, shear-wave elastography has recently been shown to be able to differentiate between symptomatic and asymptomatic tendons, Dirrichs said.
"Diseased tendons are softer than normal tendons," he said.
The researchers wanted to analyze the correlation between tendon stiffness evaluated by shear-wave elastography and clinical symptoms in symptomatic patients, as well as compare the technique's sensitivity with conventional B-mode ultrasound and power Doppler for assessing treatment response. In the prospective, longitudinal study, 35 patients with 47 symptomatic tendons received both a standardized clinical exam and an ultrasound study at three different time points: prior to therapy, after four weeks of therapy, and after six months of therapy.
The patients had a mean age of 43, and there were 20 men and 15 women. Of the 47 tendons, 17 were symptomatic Achilles tendons, 15 were symptomatic patellar tendons, and 15 were symptomatic humeral epicondylar tendons. In accordance with current orthopedic guidelines, patients were treated with a break from sports, physical therapy, and a local drug application of polidocanol ointment to the tendon, Dirrichs said.
An orthopedic specialist performed a full clinical exam at each of the three time points and assessed clinical symptoms by calculating scores based on one of three indexes for measuring disability: the Victorian Institute of Sport Assessment-Achilles (VISA-A) for the Achilles tendon, the VISA-P score for the patellar tendon, and the Disabilities of the Arm, Shoulder, and Hand (DASH) index for the humeral epicondylar tendon. The indexes calculate symptom severity on a 100-point index, with higher scores indicating higher levels of disability.
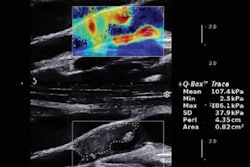
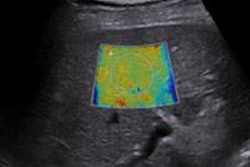
Standardized ultrasound exams consisting of B-mode, power Doppler, and shear-wave elastography were performed using an Aixplorer ultrasound scanner (Supersonic Imagine) with a high-resolution 15-MHz probe and a delay block (gel cushion), according to Dirrichs.
One of two radiologists who were experienced with sonography performed the studies, which included systematic analysis of the whole tendon and cross-sectional planes with the tendons in a relaxed state. Shear-wave elastography color maps were acquired in the proximal, middle, and distal parts of the tendon, and region-of-interest analysis of tendon rigidity was performed in three representative areas, according to the researchers. All ultrasound studies were conducted blinded to the patients' clinical symptoms and treatment.
The group then ranked each ultrasound modality's sensitivity for detecting tendon pathology at baseline as follows:
- Shear-wave elastography: 87%
- Power Doppler: 72%
- B-mode: 66%
Correlation with clinical symptoms
Beyond assessing for the presence or absence of tendon pathology, shear-wave elastography yields quantitative data that can be correlated with clinical symptoms, Dirrichs said. The shear-wave elastography values correlated closely with clinical exam scores over the course of treatment for those patients whose symptoms had improved.
Of the 35 patients, 22 had improved VISA and DASH clinical scores after four weeks and 32 showed improvement after six months of therapy. While a higher clinical exam score on the 100-point scale usually indicates a higher degree of disability, the researchers inverted the scale from 100 to 0 to make it easier to compare with the shear-wave elastography values based on kilopascals, a measurement of tissue stiffness.
| Correlation of clinical scores to shear-wave elastography values | |||
| Prior to therapy | After 4 weeks of therapy | After 6 months of therapy | |
| Inverted clinical exam score (0-100, 100 is best) | 40 | 75 | 98 |
| Shear-wave elastography values | 42 kilopascals | 64 kilopascals | 106 kilopascals |
In contrast to the very high correlation (r = 0.80) between shear-wave elastography and clinical exam scores, power Doppler findings had moderate correlation (r = 0.59) and B-mode had poor correlation (r = 0.24) with clinical exam scores.
Shear-wave elastography also outperformed B-mode and power Doppler for detecting tendon healing over therapy, according to the researchers.
| Detection of tendon healing by ultrasound modality | ||
| After 4 weeks of therapy | After 6 months of therapy | |
| B-mode-detected change in structural tendon abnormalities | 1/22 patients (4.5%) | 1/32 patients (3.1%) |
| Power Doppler-detected decrease in neovascularization | 9/22 patients (40.9%) | 13/32 patients (39.4%) |
| Shear-wave elastography-detected increase in tendon stiffness | 18/22 patients (81.8%) | 28/32 patients (90.6%) |
"[B-mode] and power Doppler had low sensitivity at baseline, so their ability to detect changes over treatment is very low," Dirrichs said. "Shear-wave elastography improves depiction of tendon healing compared with B-mode and power Doppler."