CT can detect changes accurately in regional lung volume after bronchoscopic volume reduction using a synthetic polymer sealant, according to prize-winning research presented at the 2015 annual meeting of the European Society of Thoracic Imaging (ESTI) held in Barcelona, Spain.
Minimally invasive bronchoscopic treatments are showing great promise at reducing dyspnea in patients with severe emphysema, for which there is no therapeutic option other than lung transplantation and, for a few, lung volume reduction surgery, explained Dr. Lucia Flors Blasco, who received a cum laude award from the ESTI judges for her work in this area.
 Monticello, the primary plantation of Thomas Jefferson, is still the heart of the University of Virginia.
Monticello, the primary plantation of Thomas Jefferson, is still the heart of the University of Virginia.This surgery has led to significant improvements in functional tests and quality of life in patients with predominant upper lobes emphysema, but even in experienced facilities it is associated with high morbidity (50%) and mortality (between 5% and 8% in the first 90 days after a procedure), and it is not indicated in patients with homogenous emphysema because of worse response and more rate of complications, noted Flors Blasco, an assistant professor of radiology at the University of Virginia Health System in Charlottesville, VA, U.S.
"In the attempt to achieve the benefits of lung volume reduction surgery with lesser risk and inclusion of a greater number of patients, several bronchoscopic procedures have been developed, including one-way valves, biological and synthetic polymers, thermoablation, endobronchial coils, and bronchial fenestrations and blockers," she stated in the ESTI scientific poster. "They aim for volume reduction in the pulmonary regions with severe emphysema, leading to expansion of less damaged lung and decreasing the dynamics of airway trapping."
The installation of polymers into the bronchi of emphysematous lung induces an inflammatory local reaction with posterior scarring, that collapses this parenchyma and remodels the lung. Synthetic polymers or sealant foam are formed by mixing air and a synthetic polymer (combination of amino alcohol and glutaraldehyde solutions). It blocks the interalveolar and bronchioloalveolar canals, trying to impede collateral ventilation effects seen with endobronchial valves.
Changes in lung volume
Flors Blasco set out to determine whether CT can detect changes in lung volume in patients with severe emphysema treated with bronchoscopic lung volume reduction using synthetic polymer sealant (AeriSeal), and to investigate whether these changes correlate with the clinical outcome.
Nine patients (all male, 62.7 ± 5.7 years) with advanced upper lobe predominant emphysema who underwent bronchoscopic lung volume reduction using lung sealant during an eight-month period were included in the study. All patients had symptomatic advanced emphysema not responding to treatment.
The installation of the synthetic polymer sealant was guided by bronchoscopy,under local anesthesia and sedation, according to Flors Blasco et al. Foam sealant was injected through the delivery catheter, and air was immediately introduced to produce a peripheral distribution of the product. Complete polymerization was achieved within one minute before removing the bronchoscope. A short hospital stay was required.
One or two pulmonary segments were treated per session. Some patients required an additional session to treat the contralateral lung. The treated pulmonary segment and post-treatment complications were recorded using a pulmonary function test and gasometry.
Two sessions were required in seven of the nine patients. The complications included one case each of self-limited chest pain, fever, and pulmonary abscess. All patients had paraseptal and centroacinar emphysema, and bullae were seen in five patients. CT scans after the intervention revealed the induced atelectasis of treated segments.
Low-dose chest CT
All CT scans were performed on a 64-slice CT unit (Brilliance, Philips Healthcare). The team carried out standard noncontrast low-dose chest CT exams using a 0.8 mm collimation, 1 pitch, 120 kV, and 70 reference mAs. They obtained reconstructions with 1.2-mm contiguous slices (lung reconstruction algorithm) and 2-mm slices with 1 mm-overlapping (soft-tissue reconstruction algorithm). Minimum intensity projections identified emphysema (transverse and coronal plane, slice thickness of 5-10 mm).
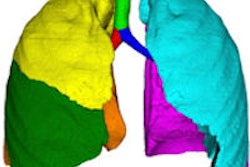
The CT scans were analyzed to measure total and lobar lung volume. Semiautomatic quantification of each pulmonary lobe was performed, and a region of interest was manually traced delineating each pulmonary lobe on axial images. Sagittal and coronal reconstructions were reviewed to verify that the segmentation followed the anatomical compartment boundaries properly. Two cases were analyzed by both observers to check for interobserver variation in the fissure-tracing technique.
The investigators retrospectively reviewed CT exams performed at baseline and 12 weeks after bronchoscopic lung volume reduction, recording treated pulmonary segment, type of emphysema, emphysema predominance, qualitative evaluation of volume loss, and presence of cavitation or pseudocavitation within the induced consolidation.
They compared the changes in the pulmonary volume within the upper lobes with the nonupper lobes (right middle and right lower lobe were considered right nonupper lobe). Qualitative volume loss was depicted in seven cases. Pseudocavities within the induced atelectasis were noted in two patients. These air-filled spaces within consolidated lung may correspond to trapped residual emphysema, air from adjacent communicated bronchi secondary to remodeling and retraction by the inflammatory tissue or sterile necrosis. These findings should not be misinterpreted as abscess, the authors pointed out.
The mild increase in volume found in the nonupper lobes (2,617.7 mL vs. 2,792.8 mL) was not statistically significant. The upper lobes significantly decreased in volume after (3,175.6 mL vs. 2,806 mL). The right nonupper lobes significantly increased in volume (1,387.6 vs. 1,527.3mL). Total lung volume did not change significantly (5,793.2 mL vs. 5,598.8 mL), they concluded.