MRI plus mammography has higher sensitivity than digital breast tomosynthesis (DBT) plus mammography, according to an article published in European Radiology. However, DBT still performs better than mammography alone and has a higher positive predictive value (PPV) than MRI.
The research team, led by Dr. Won Hwa Kim from the radiology department at Seoul National University Hospital in South Korea, studied patients who underwent mammography, DBT plus mammography, and MRI plus mammography. They found MRI has the highest sensitivity when the three modalities are compared, although it has a lower PPV than DBT.
"DBT provided lower diagnostic performance than MRI as adjunctive imaging to mammography," Kim's team wrote. "However, DBT was found to be a valuable imaging modality with higher diagnostic performance than mammography and higher PPV than MRI. If validated in larger studies, this may potentially assist the new preoperative workup in future practice."
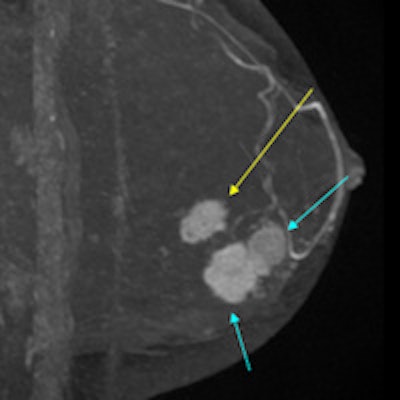
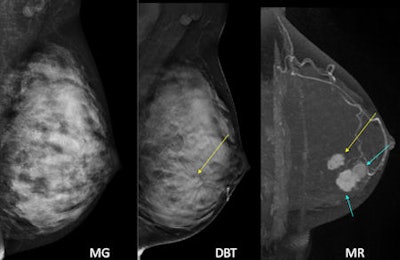 A patient with multifocal invasive ductal carcinoma. On mammography (MG) nothing can be seen. But on DBT, the mass with architectural distortion can be seen clearly. However, it was not enough; there were even larger masses in the same breast in this patient, obscured by breast density on DBT. The other masses were hard to find even in retrospect. The final pathology revealed total 4 cm extent of invasive ductal carcinoma with combined ductal carcinoma in situ. All images courtesy of Dr. Jung Min Chang, PhD.
A patient with multifocal invasive ductal carcinoma. On mammography (MG) nothing can be seen. But on DBT, the mass with architectural distortion can be seen clearly. However, it was not enough; there were even larger masses in the same breast in this patient, obscured by breast density on DBT. The other masses were hard to find even in retrospect. The final pathology revealed total 4 cm extent of invasive ductal carcinoma with combined ductal carcinoma in situ. All images courtesy of Dr. Jung Min Chang, PhD.A quest for a better modality
Mammography is an imperfect modality for detecting breast cancer, so researchers are always on the lookout for something better. MRI is highly sensitive and thus a possibility. DBT shows promise, but until now, a direct comparison between DBT and MRI has rarely been performed, and the limited data thus far have shown only comparable performance, according to Kim et al (Eur Radiol, 16 September 2015).
"We believe that comparison of DBT and MRI in terms of sensitivity, the number of false positives, and positive predictive value (PPV) is warranted at this time to widen our understanding of DBT as an emerging imaging system," they wrote.
The researchers independently reviewed image sets of 172 patients with 184 cancers. They looked at mammography alone (Selenia Dimensions, Hologic), DBT (same system) plus mammography, and MRI (Signa, GE Healthcare) plus mammography. Each image was scored for cancer probability using BI-RADS.
They found that MRI plus mammography had the highest sensitivity:
| Sensitivity and PPV by modality | |||
| Modality | Mammography alone | DBT plus mammography | MRI plus mammography |
| Pooled sensitivity | 78.3% | 88.2% | 97.8% |
| Pooled PPV | 94.5% | 93.3% | 89.6% |
Among 172 patients, the radiologists assigned only one suspicious finding in 108 patients regardless of imaging modality, and two or more suspicious findings were assigned in 76 patients for mammography alone, DBT plus mammography, or MRI plus mammography.
When the sensitivities of each modality in a subgroup of patients who had only one suspicious lesion versus patients who have two or more lesions were evaluated, overall sensitivity was significantly higher in DBT plus mammography (95.7% and 77.6%) than mammography alone in both subgroups (87.3% and 65.4%).
Sensitivity was higher with MRI plus mammography (100% and 94.7%) compared with DBT plus mammography (95.7% and 77.6%) in both groups across radiologists as well.
However, DBT plus mammography showed fewer false-positive findings and higher PPV than MRI plus mammography. There were a total of 68 false-positive findings that were assessed as BI-RADS 4A or greater by at least one radiologist on any imaging interpretation session. These lesions remained stable during the follow-up period, the researchers found.
Par for the course
"Our findings were what we expected," corresponding author Dr. Jung Min Chang, PhD, told AuntMinnieEurope.com. "We all know that MRI will have the greatest sensitivity among all modalities; however, we want to investigate the actual differences in diagnostic performance between MRI and tomo [DBT]. Also, as we expected, PPV was higher in tomo [DBT]."
DBT's inferiority in terms of sensitivity may be inherent and was, in fact, expected as DBT plus mammography is performed without a contrast agent and is, thus, unable to reflect the neoangiogenesis of malignant lesions, which can be illustrated with gadolinium-enhanced MRI, the researchers added.
"Despite the improved lesion visibility provided by DBT via reduction of the superposition of breast tissue, DBT is still an x-ray projection technique and thus cannot completely enhance a lesion perimeter obscured by surrounding tissues as shown in our results," they wrote.
At their institution, the researchers still perform preoperative MRI for patients who were diagnosed with breast cancer, said Chang, an associate professor of radiology. But in the case of patients without an MRI exam due to such factors as claustrophobia and renal failure, they recommend using DBT.
Limitations
The study has several limitations, the authors noted. The patients included were all breast cancer patients, and high-risk or average-risk women who did not have breast cancer were not included. Also, the radiologists were aware that all patients were likely to have at least one breast cancer prior to image interpretation, which may have introduced a bias, and, thus, the results may not be generalized to a screening population.
Also, the sensitivities and PPVs might not reflect the real clinical practice due to the cancer-only group and the way the statistical analysis was performed. In addition, not all lesions were surgically confirmed, and lesion verification is strictly associated with the status of test positivity, thereby potentially resulting in the overestimation of the actual sensitivity of both image modalities by reducing some false-negative lesions, they added.
"As the pathological reference was available for all the cancer cases, less than half of the benign cases were confirmed by pathological examination, even though all benign lesions remained stable during the follow-up period," the researchers wrote.
In terms of future research, Kim and colleagues are conducting more projects on DBT comparing it with ultrasound in women with dense breasts. They are also trying to investigate which patient group will most benefit from DBT.