Award-winning French researchers have produced a practical guide on how to optimize the radiation dose delivered in chest CT, focusing on reduced dose, low dose, and ultralow dose (ULD).
Iterative reconstruction methods are essential, and for an enhanced chest CT, decreasing the voltage (kV) based on the patient's morphology is the most effective way to reduce the dose, according to Dr. Marysa Schaal and colleagues from the Service de Radiologie B, Nouvel Hôpital Civil, Hôpitaux Universitaires de Strasbourg. The current optimal doses are well below the diagnostic reference levels (DRLs) of 150-250 mGy/cm for an unenhanced CT and 200-350 mGy/cm for an enhanced CT.
For an unenhanced ULD chest CT, a current of between 10 and 20 mA with a voltage of 135 kV provides a good analysis of lung parenchyma, especially for solid nodules, they noted.
A single ULD CT scan, equivalent to a radiation dose of a chest x-ray (posterioranterior and lateral) is very useful, and the proven indications are detection and follow-up of parenchymal solid nodules > 5 mm and screening of asbestos-related pleuropulmonary diseases. Other potential indications include lung cancer screening, diagnosis and monitoring of infectious pneumonia/tuberculosis, diagnosis of doubtful cases of pneumothorax, and extension of subdiaphragmatic solid tumors.
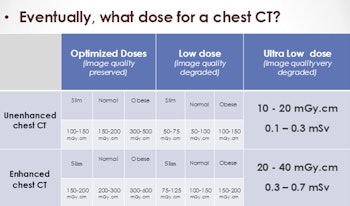
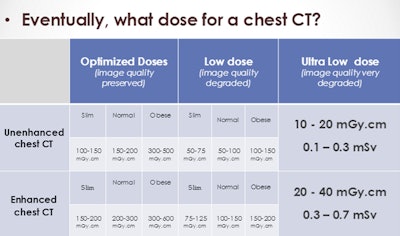
Chest CT's usual doses.
Chest CT is an excellent candidate for dose optimization, they stated in an e-poster that received a certificate of merit at RSNA 2014 and was also presented as a French-language exhibit at October's national congress of radiology, JFR 2014. Even a small dose can have a negative effect, but very low doses are likely to be harmless due to cellular repair mechanisms; in fact, low doses can have a beneficial/protective effect.
The Strasbourg team prefers the "linear no-threshold model" and precautionary principle, and stresses the importance of radiation protection, justification ("any CT examination must be clinically justified"), and optimization (ALARA, a dose as low as reasonably achievable).
The DRL in France is 475 mGy/cm (8 mSv for men, and 9.5 mSv for women). At their hospital, the level for an unenhanced scan is 2.5 to 4.3 mSv (150-250 mGy/cm), and for an enhanced scan it is 3.4 to 6 mSv (200-350 mGy/cm). Such levels are well below the legal level of radiation dose, but picture quality is optimal and well maintained.
Intrinsic factors include iterative reconstruction, dose reduction software (automatic exposure control), slice current modulation, Z-axis modulation, complex current modulation, butterfly filter, and collimation. Extrinsic factors comprise voltage, charge, and pitch. "We can intervene on these," noted the authors.
Iterative reconstruction is the cornerstone of ULD CT and the successor to filtered back projection. It allows indirect dose reduction thanks to physical models designed to reduce noise and artifacts, and many studies have shown that iterative reconstruction maintains, if not increases, the unenhanced chest CT's image quality, while reducing radiation dose, they continued.
"Reducing the voltage means reducing the flow of photons coming out of the tube. As the radiation dose varies with more than the square of the voltage, it is a very efficient means to reduce irradiation, as long as explored volume remains small (children or adults with low body mass)," Schaal et al wrote. "Voltage reduction has also the capability to increase iodine contrast, thanks to a photoelectric effect increase."
The charge -- i.e., the product of the current (applied at cathode) by the time -- represents the quantity of photons emitted, and therefore the dose is proportional to it. The noise increases when charge decreases, but this parameter is rarely modified directly because the automated current (or charge) modulation systems control it according to the explored anatomical region, so as to keep the signal-to-noise ratio (SNR) constant, they explained.
In the case of the Z-axis modulation, current intensity is modulated according to patient body shape and density variations. The current is therefore higher for obese patients, and at the abdominal or pelvic level rather than at the chest level. The latest software can manage current modulation at each slice based on volume mitigation determined at the previous slice altogether with scout measures, according to the researchers. The operator can control the quality level of the examination according to an acceptable SNR, and the current is then defined automatically and dynamically to ensure homogeneous image quality.
Pitch is the distance achieved by the table in one revolution divided by the slice thickness, and exposure can be reduced by increasing the pitch (> 1) as x-rays absorbed are inversely related to the pitch. On a single-source CT, the pitch can be increased to 1.5 without noticeable data loss, but with a dual-source CT, pitch can be increased up to 3.6, they wrote. Higher pitch means reduced exam time and can be useful for patients with breathing difficulties or for cardiac CT. Nevertheless, the pitch is rarely modified because increasing it implies a higher noise level and more artifacts in the Z-axis if all the other parameters are not adjusted accordingly.
| Chest CT's usual doses | |
| Investigated region | EDLP conversion coefficient |
| Head | 0.002 |
| Abdomen and pelvis | 0.015 |
| Chest (male) | 0.017 |
| Chest (female) | 0.020 |
For enhanced chest CT, decreasing the voltage (kV) is the most effective way to reduce the dose, and it may be feasible to reduce the tube voltage to 100 kV for patients with a body mass index (BMI) of less than 23, or even to 80 kV for those with a BMI of less than 20. Research shows the dose can be reduced by 44% using 100 kV instead of 120 kV, with no loss of quality, and some 80 kV protocols have shown a dose reduction of 36% to 52% with no CNR alteration, the authors noted. These protocols are not appropriate for patients more than 100 kg or obese, and in such cases, it is better to use 120 kV and slightly reduce the quality index (noise level).
For unenhanced chest CT with optimized dose, it is advisable to systematically reduce voltage down to 100 kV, unless the BMI is more than 35.
ULD chest CT is valid for the detection and the follow-up of solid nodules (> 4 mm), and ULD chest CT performances are weaker for the detection of semi-solid or ground-glass nodules, especially if they are smaller than 5 mm, they continued.
For lung cancer screening, ULD CT is probably excellent, with very good sensitivity for detecting nodules and very low radiation exposure, which is really important in the context of screening, but it has yet to be proven for detecting asbestos-related pleuropulmonary diseases, the authors wrote. ULD CT can perform well at an effective dose16 times lower than that of a standard CT acquisition (0.3 mSv versus 4.9 mSv), and can be a front-line screening test, with full dose acquisition used only in doubtful or positive cases. This would allow a reduced radiation dose of nearly 75% for the screening population.
Among the future applications of ULD are exploration of febrile neutropenia and especially fungal infection in immunocompromised patients, lymphoproliferative diseases with repeated CT, evaluation of patients with cystic fibrosis, CT-guided biopsy of pulmonary lesions, and extension of subdiaphragmatic tumors. ULD has limitations, however, particularly for obese patients and in cases of ground-glass pulmonary opacities and inconspicuous interstitial abnormalities, they concluded.