Researchers in Switzerland and the U.K. have built a computer-aided detection (CAD) system that locates and measures peripheral artery disease (PAD) based on the size of the lumen and the degree of stenosis. The system has been tested on a phantom and in 15 patients, where it yielded an accuracy of 88% for detecting stenosis, along with a low false-positive rate.
More than simply CAD to detect stenosis of the peripheral vessels, the system includes a computer-aided-measurement (CAM) component to measure the artery diameters from the detected vessel centerline, using an expectation maximization function to compensate for partial-volume effects.
"The results demonstrate the potential application of CAD-CAM for PAD, which we believe can be further improved using more sophisticated algorithms for determining the degree of vessel narrowing in stenosis," wrote Jamshid Dehmeshki, PhD, professor of medical image analysis in the Faculty of Science, Engineering, and Computing at Kingston University, U.K., along with colleagues from the University of Lausanne (Studies in Health Technology and Informatics, 2014, Vol. 205: e-Health - For Continuity of Care - Proceedings of MIE2014, p. 1153-1157).
PAD is a serious health concern that is growing in scope with the aging of the population. On the diagnostic side, CT angiography of the peripheral arteries is a reliable way to detect stenosis, vessel occlusion, and calcification, noted the authors.
The problem is that CT images are degraded to some extent by the presence of partial volume effects, which present a difficult-to-decipher blend of CT intensities at the vessel boundary voxels and surrounding tissues. Inhomogeneous bone tissue, image noise, and as many as 1,000 slices per scan further complicate image analysis. Therefore, a system capable of detecting and quantifying peripheral artery stenosis reliably is a valuable goal that has eluded developers.
Researchers have done their footwork in the form of various techniques for segmenting the peripheral vessels, notably by Petr Felkel, PhD, and colleagues from Prague and Vienna, who identified issues such as nonhomogeneous distribution of contrast and partial volume effects, according to the authors.
"However, most of their approaches require manual intervention," Dehmeshki et al wrote. A system has been created for vessel visualization and analysis in MRI, but detection analysis was limited and not focused on peripheral arteries.
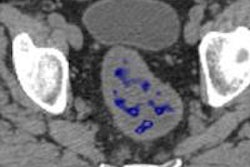
The CAD-CAM system proposed in this paper automatically detects peripheral arteries using image segmentation operations including optimal thresholding, 3D region growing, and bone removal, the study team wrote. The system also offers fast morphology operations, artery centerline detection, and distortion correction. Accurate measurement of the artery diameters is performed orthogonal to the centerline and is combined with a method to compensate for the partial volume effect based on Expectation Maximization (EM) and Markov Random Field (MRF).
As for the CAM or vessel measurement piece, the authors noted it has been explored in the literature previously, but only in general applications of vascular measurement and on a 3D phantom that represented vessels with different structures.
Under the hood
This paper proposes an integrated, automated CAD-CAM system for detecting PAD, combining several elements:
Optimal thresholding. This process uses intensity thresholding to detect high-constrast vessels in CTA images. Threshold values are estimated using optimal selection algorithm.
3D region growing. The 3D region-growing algorithm is initiated at a location determined by identifying the bifurcation of the aorta, where it joins with the common iliac artery.
Bone removal. This persistent problem in the pelvic and popliteal regions is tamed with a bone removal algorithm. First, a connected component analysis algorithm is used to label the image in 2D and 3D regions, and the algorithm uses anatomic spatial and anatomic data for problematic anatomic regions. For example, the authors note the algorithm uses the large size of the pelvic bone as an identifying characteristic to detect and remove it. A morphology operator function detects and removes gaps in image connectivity.
Centerline detection. This process uses a thinning algorithm that deploys a fast symmetrical erosion technique based on topological information of the image. The algorithm finds all of the detectable surface points based on a decision-tree method.
Orthogonal plane construction. In this process, image cross-sections are obtained from a slice-based rendering technique that relies on texture to visualize 3D datasets, and represent them as a 3D texture.
Vessel diameter measurement. The measurement is performed directly from the orthogonal image cross-section and computed as the diameter of a circle. An algorithm based on maximum a posteriori (MAP) expectation maximization is used to compensate for the partial volume errors.
Stenosis identification is the last step, based on a distinctive narrowing of the vessel diameter over a short length of vessel, the authors reported.
CAD-CAM versus conventional thresholding
In a vascular phantom experiment, the MRF-MAP method was compared with conventional thresholding at 200 HU. In 32 phantom samples of 18 slices each, the results showed that MAP-MRF was superior to the threshold algorithm, resulting in significantly smaller errors for the estimation of vessel diameters.
| Threshold versus MAP-MRF method in CAD-CAM | ||||
| Vessel diameter (mm) | 1 | 2 | 4 | 6 |
| Threshold % error | 32% | 26.6% | 15.9% | 11.3% |
| MAP-MRF % error | 11% | 6% | 7% | 7% |
In 15 patients, CAD-CAM methodology was applied to 15 patients with PAD who had undergone CT imaging on a multislice scanner (GE Healthcare) using 0.6-mm slice thickness. Applied to 149 stenotic vessel segments, CAD-CAM yielded 88% sensitivity with a specificity of 96% (three false-positives), according to the authors.
When CAD-CAM was applied to CTA patient scan data, it was able to detect 131 stenosis locations compared with the 149 reported by a radiologist with a false-positive rate of only 4%.
"These results are particularly promising as, according to the radiologists' assessment, 132 of the stenoses can be attributed to soft plaque deposits, which can be more challenging to detect than the hard plaque variety," they wrote. "The results demonstrate the potential application of CAD-CAM for PAD, which we believe can be further improved using more sophisticated algorithms for determining the degree of vessel narrowing in stenosis."