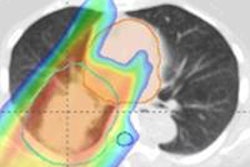
The fine-tuning of proton therapy plans to maximize tumor dose and minimize dose to healthy tissue is held back by significant uncertainties in the stopping power estimates used to calculate proton range. The stopping powers are derived from the Hounsfield units in x-ray CT scans of the patient and their uncertainty arises from a lack of one-to-one mapping between the two parameters.
Now, researchers in Denmark have improved the accuracy of stopping power estimates with a dual-modality image reconstruction (DMR) technique that combines x-ray cone-beam CT (CBCT) data with a proton CT scan (Medical Physics 2014, Vol. 41, pp. 031904).
"For a range of patients, DMR would allow for better stopping power estimates than could be obtained with standard x-ray CT or proton CT alone," said first author David Hansen, a physicist at Aarhus University. "This in turn would allow for more accurate particle therapy, hopefully translating into better clinical outcome for the patients."
 Aarhus University researchers, left to right: Thomas S. Sørensen, Niels Bassler, David C. Hansen, and Jørgen B.B. Petersen. Image credit: Michael Harder.
Aarhus University researchers, left to right: Thomas S. Sørensen, Niels Bassler, David C. Hansen, and Jørgen B.B. Petersen. Image credit: Michael Harder.DMR corrects the x-ray-based CBCT stopping power estimates using the proton data. It does so by identifying regions in each scan that have similar stopping powers on the basis of a statistical weight that quantifies the confidence in the CBCT stopping power estimates.
Simulating proton CT
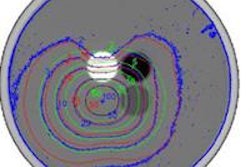
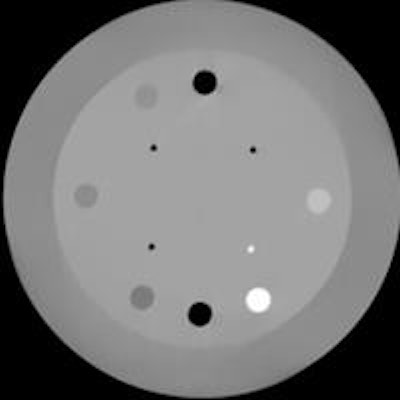
The researchers tested DMR using Monte Carlo code to simulate 230 MeV proton CT scans on a digital version of a cylindrical phantom. The simulated scans detected the entry and exit position and momentum of every proton, collecting data over 360° around the phantom using two opposing detectors. A physical x-ray CBCT scan of the same 15-cm diameter phantom was acquired using an on-board kilovoltage imager on a conventional linac.
While one proton scan was reconstructed using the full 360° dataset, Hansen and his colleagues also mimicked scans with incomplete sampling, assessing the benefit of DMR where proton range is less than the patient thickness in a given direction. The scenario will arise for treatment sites other than the head, given a 230 MeV beam -- the highest energy typically produced by commercially available proton therapy systems -- has an approximate range of 33 cm.
When 360° sampling was used, proton CT and DMR consistently provided markedly more accurate stopping power estimates than x-ray CBCT, with a mean RMS error of 0.003 across a range of phantom insert materials. In one example, the RMS error for a polystyrene insert, which has a reference stopping power value of 1.03, was approximately 11 times smaller for DMR and proton CT compared with CBCT.
Reduced sampling retains benefits
Reducing the angular sampling of the proton CT data with two opposing sectors, each 90° wide in one DMR scan, and 45° in another, also reduced the accuracy. However, the technique was still more accurate than CBCT in isolation. For the same polystyrene insert, DMR was between 1.5 and 3.5 times more accurate than CBCT. For the 45° sectors, there was a marked deterioration in DMR spatial resolution compared with the fully sampled case, but this was avoided with the 90° sectors.
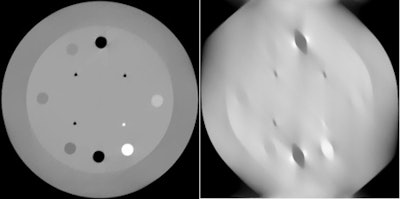 Dual modality reconstruction (DMR), (left) and proton CT (right) achieved improvements in stopping power accuracy over x-ray CBCT. These images were reconstructed using proton CT scans of the phantom that sampled two opposing 45° sectors.
Dual modality reconstruction (DMR), (left) and proton CT (right) achieved improvements in stopping power accuracy over x-ray CBCT. These images were reconstructed using proton CT scans of the phantom that sampled two opposing 45° sectors.Hansen told medicalphysicsweb that the findings are encouraging. "Proton CT might be of benefit for particle therapy, even when it's not possible to scan from all angles," he said.
An additional advantage of the DMR approach is that proton and CBCT scans -- the latter acquired using on-board imaging -- can be obtained simultaneously while the patient is on the treatment couch. This avoids the geometrical errors associated with scanning at different times, between which patient anatomy and positioning may change. The technique can also be adapted to correct megavoltage and kilovoltage x-ray CT and MRI scans.
The researchers are currently in talks with groups at Loma Linda University in California and Ludwig-Maximilians University in Munich to arrange testing of DMR on prototype proton CT scanners that these groups are developing.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.