MR-guided focused ultrasound (MRgFUS) has the potential to become one of the most exciting and revolutionary treatment technologies of the 21st century, according to presenters at an ECR 2014 scientific session. They highlighted the technique's capability to improve treatment of a wide range of medical conditions.
In clinical trials, and in countries where regulatory approval has been obtained, focused ultrasound is being used to treat uterine fibroids, liver tumors, and functional neurological disorders, such as essential tremor, neuropathic pain, and tremor-dominant Parkinson's disease. It is being used in lieu of conventional external-beam radiotherapy to deliver palliative treatment for painful bone metastases. Preclinical laboratory testing of image-guided FUS-activated delivery of highly toxic chemotherapy drugs to combat brain cancers is also underway, with the expectation of clinical trials starting in this decade.
Dr. Chrit Moonen of the University Medical Center Utrecht in the Netherlands explained to ECR delegates how FUS precisely concentrates converging beams of ultrasound energy onto a target as small as 1 mm in diameter deep within the body. Deposition of a high level of ultrasonic energy causes an intense increase in temperature, thermal coagulation, and cell death. MR guidance allows in situ target definition and identification of adjacent healthy tissue to be spared. MRI can also provide continuous temperature mapping during treatment, for spatial and temporal control of the heating procedure and prediction of the final lesion based on the received thermal dose.
Uterine fibroids
The earliest and most commonly used FUS application is treatment of symptomatic uterine fibroids. The procedure was first introduced in 2003, and has now received regulatory approval in Europe, Australia, the U.S., India, Japan, and Australia. For many women, it is a viable alternative to hysterectomy, not only preserving the potential for reproductive function, but also eliminating the lengthy and detrimental recovery associated with major abdominal surgery. The procedure is ambulatory outpatient surgery, and women typically recover within a day or two, compared with weeks of curtailed activities and potentially months to full recovery.
Session moderator Dr. Wladyslaw Gedroyc, the medical director of MRI at St. Mary's Hospital in London, said it is truly unfortunate that this procedure is not recommended by more gynecologists and covered as routinely as hysterectomies by insurance companies. "The procedure is no more expensive than performing a hysterectomy. The improved quality of life for a patient having FUS treatment for uterine fibroids is so much better than having a hysterectomy. And from a strictly economic standpoint, a patient can rapidly return to earning wages."
He recommends that radiologists take a more active role in educating gynecologists about MRgFUS. He observed that too often he hears anecdotally that it is the patient who educates a gynecologist, not the gynecologist educating the patient about this alternative and potentially healthier option.
Transcranial FUS
Transcranial FUS is a much newer, novel technique for noninvasive neurosurgical interventions using no ionizing radiation. Using large phased-array transducer technology and skull bone modeling, MRgFUS integrates transcranial FUS with MRI for target definition, treatment planning, and high-precision intervention guidance, while simultaneously monitoring energy deposition in the target tissue and the resulting temperature progression in real-time. The ability to visually follow the surgical lesion online can minimize the danger of mistargeting and causing serious side effects. The risk of serious late adverse effects caused by irradiation to the brain also is eliminated.
Dr. Ernst Martin-Fiori of the University Children's Hospital in Zurich has been using this technology since 2006. He and his colleagues have treated a variety of chronic, therapy-resistant neurological diseases with high-intensity FUS to the thalamus, subthalamus, or basal ganglia. He noted that ongoing clinical studies at various centers on more than 130 patients with neuropathic pain, essential tremor, Parkinson's disease, and obsessive compulsive disorder are very encouraging.
The University Children's Hospital expects to treat about 40 adult patients this year, a number that has increased since the equipment used (ExAblate Neuro, InSightec) received CE Mark approval in December 2012. "Patients come from all over the world. We perform about one intervention a week, and we have a waiting list," Martin noted. "The results for many patients with serious, chronic essential tremor can be remarkable. The effect of reducing or eliminating tremor is immediate. For these patients, this procedure is life-changing." The cost is about 30,000 to 35,000 Swiss francs (24,650 to 28,750 euros).
The outcome for patients with pain, particularly paraplegic patients who are experiencing phantom pain from amputated limbs, is dependent upon their personality. Results of a recent clinical study showed that average pain relief experienced by 18 pain patients ranged between 48% and 57% (Parkinsonism & Related Disorders, January 2014, Vol. 20:suppl 1, pp. S197-S199). The euphoria experienced from improvement -- eliminating morphine and pain-killing drugs, easier mobility, and less physical and mental suffering -- diminishes over time, according to Martin. "A year later, many patients express dissatisfaction with outcomes, but if you ask their spouse or caretaker, that person will have a much more positive opinion."
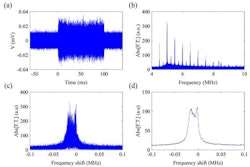
Martin also discussed new preclinical animal studies that combine transcranial MRgFUS with microbubbles to open the blood-brain barrier for treatment of glioblastoma. Researchers are encapsulating highly toxic substances and chemotherapy drugs into nanoparticles -- drugs that would seriously harm the patient if administered intravenously. Ultrasound can be used to open the blood-brain barrier at the desired treatment location, enabling the toxic agents to work only and exactly where they are needed.
"A lot of neuropharmaceutical agents that are also used as chemotherapy agents are too large to penetrate the blood-brain barrier. Only about 1% of the applied dose given intravenously is reaching the brain," Martin said. "A lot of brain tumors today, as well as neurodegenerative diseases, are being suboptimally treated because it is not feasible to deliver the concentration needed for tumor eradication. Transcranial MRgFUS has the potential to change this."
Clinical trial protocols are currently being developed for patients with breast cancer metastases to test how well this type of treatment works. "If we could open the blood-brain and the blood-tumor barriers to get the drug into the brain metastases, maybe we could save a lot of lives. Transcranial MRgFUS promises new therapeutic approaches for a variety of diseases that have the potential to change patient management," Martin said. He and many other radiologists, neurologists, oncologists, neurosurgeons, medical physicists, and other clinicians are very excited about the potential of this technology.
Cynthia E Keen is a freelance journalist specializing in medicine and healthcare-related innovations.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.