
Using digital chest tomosynthesis in patients with suspected thoracic lesions decreased per-patient diagnostic imaging costs, resulting in approximately 8,000 euros saved per year, and reduced the need for a CT scan by nearly 75%, according to a new study by Italian researchers.
Detecting and characterizing pulmonary lesions, particularly pulmonary nodules, on chest radiography (CXR) is challenging, because of their frequently small size and poor conspicuity within surrounding anatomical structures. Pulmonary lesions are often visible only retrospectively when reviewing previous radiographic images of patients with known nodules, and computer-aided detection (CAD) systems have been advocated to improve the diagnostic accuracy, according to Dr. Emilio Quaia, from the radiology department at Cattinara Hospital, University of Trieste in Italy, and colleagues.
"Frequently, the radiologist reporting CXR identifies doubtful or equivocal findings that could be referred to as both pulmonary and extrapulmonary lesions, or also as pulmonary pseudolesions because of different planes overlapping or composite areas of increased opacity," they wrote in a study published in Insights into Imaging (14 January 2014).
Thus, CT is primarily the gold standard for imaging pulmonary lesions, but it is expensive, delivers a considerable radiation dose to the patient, and the diagnosis time also can be longer because of CT unit work overload. Enter digital tomosynthesis.
Compared with CXR, digital tomosynthesis produces superior images for identifying the intra- or extrapulmonary lesions previously suspected based on initial CXR interpretation. It also removes overlying anatomical structures, enhances local tissue separation, and provides more depth of information of the structure of interest. And it has a lower radiation dose than CT.
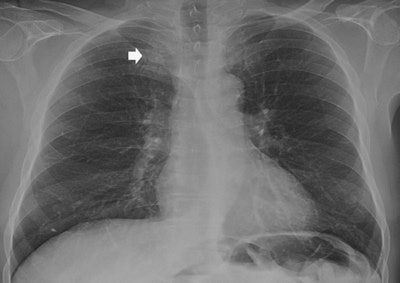 A 65-year-old man with a peripheral pulmonary ground-glass pulmonary nodule. Above: Posteroanterior chest radiography in the upright position shows one suspected pulmonary opacity of the apex of the right lung (arrow) behind the overlying anterior arch of the first right rib. Below: Digital tomosynthesis planes show a ground-glass pulmonary nodule (arrow) with evidence of intralesional air bronchogram. All images courtesy of Dr. Emilio Quaia.
A 65-year-old man with a peripheral pulmonary ground-glass pulmonary nodule. Above: Posteroanterior chest radiography in the upright position shows one suspected pulmonary opacity of the apex of the right lung (arrow) behind the overlying anterior arch of the first right rib. Below: Digital tomosynthesis planes show a ground-glass pulmonary nodule (arrow) with evidence of intralesional air bronchogram. All images courtesy of Dr. Emilio Quaia.
Digital tomosynthesis could be considered a problem-solving technique in patients with suspected pulmonary lesions on CXR, and could be used in place of CT in this particular clinical setting. However, until now, no previous studies evaluated the actual impact in diagnostic imaging costs before and after digital tomosynthesis implementation.
Quaia and colleagues did just that in their study, which included 465 patients (263 men, 202 women) with suspected thoracic lesions. Each of the patients underwent digital tomosynthesis after CXR. Each patient also had a CT exam when a pulmonary noncalcified lesion was identified by digital tomosynthesis -- CT was not performed when a benign pulmonary or extrapulmonary lesion or pseudolesion was identified.
The average per-patient imaging cost was calculated by normalizing the costs before and after digital tomosynthesis implementation.
In 229 of 465 patients who underwent digital tomosynthesis after suspicious CXR, digital tomosynthesis showed 193 pulmonary lesions and 36 pleural lesions. In the remaining patients, lesions were ruled out as pseudolesions on CXR.
A chest CT exam was performed in 127 (27%) patients, while in the remaining 338 (73%), CXR doubtful findings were resolved by digital tomosynthesis, meaning nearly 75% of patients were able to avoid a chest CT exam.
The average per-patient costs of CXR, digital tomosynthesis, and CT were 15.15 euros, 41.55 euros, and 113.66 euros, respectively. Digital tomosynthesis allowed an annual cost savings of 8,090 euros considering unenhanced CT and 19,298 euros considering contrast-enhanced CT. Using a digital tomosynthesis reimbursement rate of 62.7 euros, the breakeven point corresponds to 479 digital tomosynthesis exams, according to the researchers.
The study results suggest that digital tomosynthesis may confirm or rule out pulmonary lesions and pseudolesions and also differentiate true pulmonary opacities from those due to pleural or thoracic wall lesions with a clear improvement in diagnostic accuracy, confidence, and interreader agreement in comparison with CXR and with a modest increase in the radiation dose and interpretation time, the authors wrote.
"This presents a strong clinical impact, since up to 20% of suspected nodules on CXR can be entities mimicking a solitary nodule," they wrote.
The study also shows the per-patient diagnostic imaging costs decreased after digital tomosynthesis implementation in patients with suspected thoracic lesions. This was mainly due to the "dramatic effect" of digital tomosynthesis on the CT utilization rate that decreased significantly after digital tomosynthesis implementation, they noted.
"According to these results, DTS [digital tomosynthesis] may be considered a first-line problem-solving imaging technique to rule out pulmonary lesions," Quaia and colleagues wrote. "Low-radiation-dose chest CT could represent an alternative imaging modality, even though it appears more suitable for lung cancer screening, while the advantage of DTS is the verification of doubtful findings directly in the x-ray unit without moving the patient to CT and with a comparable effective dose to CXR and low-radiation-dose CT."
Limitations
Compared with CT, the main limitation of digital tomosynthesis is the limited depth resolution caused by the limited tomographic sweep angle. In this study, all findings misinterpreted at digital tomosynthesis were subpleural or located in the region of the lung in the proximity of the chest wall, where the limited depth resolution of digital tomosynthesis may hamper the correct spatial location of the findings.
"This limitation is related to the geometric frontal plane acquisition by DTS, since acquisition in the sagittal plane is not recommended because of the higher dose exposure," the researchers wrote.
Also, digital tomosynthesis studies took longer to read than CXR mainly because of scrolling through multiple images, but the overall interpretation time was lower than CT because of the lower number of images evaluated.
"Even though DTS increased the interpretation time, it could be easily introduced in the routine diagnostic work flow as a case-solving technique in those patients with suspected or equivocal pulmonary lesions on CXR," the researchers wrote.
All costs were calculated based on a single hospital and are not necessarily transferable to other settings because of the difference in valued added tax (VAT) and personnel wages in Italy.
In an interview with AuntMinnieEurope.com, Quaia said he plans to write a paper entirely dedicated to cost analysis that does not include VAT calculation.
"DTS could be interesting in a decentralized setting (e.g., Northern European countries) where small sites would not have a CT scanner," the researchers wrote. "In this case, a digital x-ray unit could allow a further sparing by clarifying unclear pulmonary lesions without having the patient traveling far to the next center with CT equipment."
The main limitation of Quaia and colleagues' study is the inclusion of a heterogeneous group of patients who underwent CXR for different clinical reasons. The inclusion of a more selected patient cohort (e.g., patients with suspected pulmonary nodules or patients with a known primary tumor and suspected lung metastases) could provide further insights into the diagnostic accuracy and cost analysis of digital tomosynthesis, they noted.
Another limitation is the absence of blinded evaluation of CXR and digital tomosynthesis images, because this prospective study was part of routine medical care.
Finally, the presence of multiple reference standards, including CXR for pseudolesions or overt benign lesions and CT or histology for positive pulmonary lesions, is a limitation.
"This is because we decided to spare those patients who did not present any finding deserving further imaging workup on DTS from a CT dose, and because this actually represents what usually happens in routine clinical practice," they wrote.
In Italy, digital tomosynthesis is being implemented in more institutions, although its availability is not widespread, Quaia said. There are roughly seven Italian centers that have this technique.



















