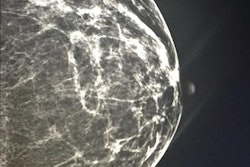
Harmonization and best practices in mammography would benefit from more detailed guidance, Portuguese researchers have found. They reached this conclusion after reviewing quality assurance (QA) guidance documents from around the world.
There have been several guidance documents for mammography QA in the past 20 years, but the scope has focused on technical aspects, whereas other specialties -- such as epidemiology, interventional, pathology, and surgery -- have added an emphasis on clinical aspects. Due to the developments in digital mammography over the past 10 years, QA programs have sprung up along with a need for new tests and procedures for quality control (Insights into Imaging, 4 August 2013).
QA provides a framework for constant improvement through a feedback mechanism. It also identifies deviations from optimum performance of mammographic equipment, suboptimal clinical practice, and training needs.
"An effective QA program should be practical to implement in a clinical setting," wrote lead author Cláudia Reis, from the Lisbon School of Health Technology (ESTeSL), and colleagues. "Adequate test equipment is necessary as well as standard methodology that provides [the] ability to obtain the relevant objective, and subjective metrics of quality. Also, an effective QA program should be implementable at a low or moderate cost."
Reis and colleagues identified, analyzed, and compared selected protocols currently available for QA in mammography, and they discussed the protocols' contribution to harmonize practices in mammography worldwide.
The researchers performed a literature search to identify guidance documents available from international bodies, healthcare providers, and professional/scientific associations. The guidance documents were reviewed and compared for type of guidance (clinical/technical), technology, and proposed QA methodologies focusing on dose and image quality (IQ) performance assessment.
Fourteen protocols (targeted at conventional and digital mammography) were reviewed. All of them included recommendations for testing acquisition, processing, and display systems associated with mammographic equipment. All guidance highlighted the importance of dose assessment and testing automatic exposure control (AEC) on mammography systems. Recommended tests for assessment of image quality showed variations in the proposed methodologies and focused on assessment of low-contrast detection, spatial resolution, and noise.
What's the best guidance?
The International Atomic Energy Agency (IAEA) digital mammography protocol (edited 2011) is the most up-to-date guidance and is dedicated to digital mammography, Reis and colleagues found.
The U.K./Institution of Physics and Engineering in Medicine (IPEM), European Commission (EC), IAEA, and American College of Radiology (ACR) protocols are well-established documents originally developed for film-screen mammography that have been adopted in many countries worldwide.
The EC guidelines were updated and an addendum on digital mammography was included. An updated version of the ACR protocol is known to be in progress to include guidance specifically targeted at digital mammography, the authors acknowledged. Also, according to information available on the European Reference Organization for Quality Assured Breast Screening and Diagnostic Services (EUREF) website, a revised edition (fifth) of the EC guidelines is in development.
The EC and Irish protocols are wider in scope and may be useful to a broader range of healthcare professionals. Other protocols focus on dosimetry and image quality assessment and are targeted at medical physicists, radiographers, and breast radiologists.
What should be tested?
All protocols reviewed recommend testing the x-ray source (tube voltage and half-value layer) and the AEC system.
"AEC testing is one of the most important procedures due to its direct impact on IQ and breast dose," Reis and colleagues wrote. "It should consider the effects of variations in object/attenuator thickness and radiation beam quality."
The recommended methodologies for breast dose estimation vary. Measurements using test objects and breast phantoms are frequently recommended and more practical to implement than measurements based on thermoluminescent dosimeter (TLD) techniques, they wrote.
Dose assessment with a standard test object/phantom allows the comparison of different mammographic techniques and the investigation of the effect of technical settings on breast dose. Clinical dose assessment provides valuable information on the clinical practice and takes into account the influence of breast thickness and composition on dose.
All guidance documents recommended performing low-contrast threshold detection testing, breast lesion visualization (e.g., simulated in phantoms), and artifact analysis. Compression force, image noise, and spatial resolution testing were also recommended with variations in the proposed methods and test materials.
The EC protocol recommended assessment of image quality of digital mammographic systems using images produced with a specific low-contrast-detail test object (CDMAM), which is a costly tool that is not readily available in all imaging departments, the researchers wrote. The U.K./IPEM and ACR protocols recommend alternative test objects to CDMAM, namely TOR (MAM) and the ACR accreditation phantom.
"Despite the potential critical impact of image processing in the quality of the final image, the testing of image processing tools is still at early states (compared with testing of hardware)," Reis and colleagues wrote.
Most protocols recommend testing based on raw image data and do not include recommendations for testing postprocessing algorithms used in clinical images.
"Establishing testing protocols for postprocessing tools in digital mammography is a challenging task as processing tends to be manufacturer specific and frequently manufacturers are reluctant to reveal details of the postprocessing algorithms incorporated in their systems," they added.
Also, reference values and acceptability criteria vary between protocols, which raises the question of whether it would be possible to have a mammography system complying with a test procedure and acceptability criteria, whereas using another test procedure the system would fail, they wrote.
Selection criteria should take into account resources and expertise as well as the relevance of the tests to local practices, they noted.
"A key factor to promote the success of a QA program for mammography is teamwork and the collaboration of all key staff (e.g., radiographers, radiologists, medical physicists, and healthcare managers)," the group wrote. "Training and continuous feedback mechanisms are essential to improve the testing procedures and strengthen the outcomes of the program."
If professional networks and special interest groups exchanged experiences with colleagues worldwide it could be invaluable in the initial phases of implementation of a mammography QA program, the authors concluded.