Mammography using conventional x-ray remains the industry standard for breast cancer screening, but ongoing concern over radiation dosage, combined with the diagnostic limitations of the standard procedure, has prompted a long-term search for a viable alternative. This search has been further hindered by ongoing confusion, debate, and variance in standards of mammography equipment use as a screening tool.
The first contender in the search is ultrasound, a modality overlooked by many due to the apparent limitations in image quality and user expertise required. Yet, recent advances in automation and resolution, and the emergence of dedicated breast sonography systems, are changing this view.
At present, ultrasound is typically used to supplement mammography in detecting tumors that may not be visible with mammography alone. Use of elastography to "type" cancer is increasingly common, assisting in prediagnosis before biopsy. While advances in elastography now allow tumor stiffness to be measured, a lack of harmonization on the measurement scale used, and limited automation, has hindered the promotion of ultrasound as a strong candidate.
Incidence and Mortality Rates of Female Breast Cancer
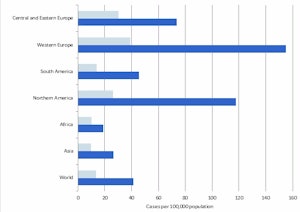
Click image to enlarge graph.
However, ultrasound is less affected by breast density compared with conventional mammography, an increasing challenge for healthcare providers, especially in the proliferating Asia-Pacific region. A recent study by the American College of Radiology Imaging Network (ACRIN) and University of Pittsburgh School of Medicine found that additional ultrasound screening following mammography increases the chance of finding invasive breast cancer in women with dense breasts.
Despite this, ultrasound is still some way off being used as a standalone screening tool for breast cancer. Automated breast volume sonography (ABVS), released in the last few years, could be the first step. Another study, by the Bangkok Breast Center, has shown that ABVS significantly improved the detection of breast cancer in Asian women compared with handheld ultrasound. With ABVS, the field-of-view is larger and the exam provides reproducible and standardized images. Further studies have also shown that ABVS is time-efficient and could be easily used in a screening environment.
A number of challenges still remain for ultrasound. While the technology has made significant advances in cancer detection and typing, a lack of a harmonized automated measurement scale, and no large-scale clinical trial evidence, has prevented ultrasound from being used as a front-line primary screening tool. Therefore, despite advances in dense breast screening, more assurance must be provided or it will continue to be used alongside mammography instead of as a replacement.
The search for a viable alternative also led to equipment developers looking closer to home, adapting and optimizing conventional mammography. Tomosynthesis has been the highest profile of such advances, especially following the long-awaited approval of the first tomosynthesis system by the Food and Drug Administration (FDA) in the prominent U.S. market.
Tomosynthesis involves the construction of a 3D mammography image, allowing radiologists to pan through the image. One of the key challenges in conventional mammography is discerning between cancerous tissues and "shadowing" caused by tissue overlap when compressed. Tomosynthesis allows wider, multiplane investigation of these areas, increasing the quality of the diagnosis and minimizing false negatives, highlighted by a number of small-scale clinical trials recently released.
Yet, tomosynthesis is not the perfect solution for screening. Ignoring the additional cost of the tomosynthesis, the current technology increases the radiation dose administered, albeit, not substantially. However, mammography legislation and standards are one of the most widely debated and contested, so further cause for concern may limit uptake. Interestingly, a new concept proposed by women's imaging vendor Hologic is aiming to reduce radiation dose, utilizing the tomosynthesis concept to fuse low-dose images together. This "compound view" would eliminate the need for an initial higher dose 2D image to be made, and reduce the total dose administered. While clearly a progression on standard tomosynthesis, the fickle and complicated approval process may limit widespread use for some time.
Adaptive Pathway for Breast Screening - Breast Density Basis for Adaptive Diagnosis Pathway
','dvPres', 'clsTopBtn', 'true' );">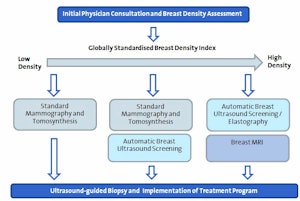
Click image to enlarge chart.
Advanced imaging also is being considered following increasing evidence and use in breast cancer diagnosis. Molecular breast imaging has so far provided the strongest argument for wider clinical use. This technique uses tracing agents to measure the molecular activity of tissues within the breast, rather than measuring the density of tissues, eradicating the problem of screening in dense breast tissue. Yet, while the specificity of this approach allows accurate typing and identification of malignant and cancerous tissue, it comes at a cost, both financially and in terms of patient safety. To monitor molecular activity, radioactive tracers must be used, albeit in small, limited doses. While the risks are relatively low for a single scan, repeated screening may not be feasible. Furthermore, the high-cost of MRI equipment may also act as a barrier to widespread screening, particularly in emerging or rural regions where access to advanced imaging services is scarce.
All of the above developments are significantly advancing the specificity and quality of breast cancer diagnosis. Yet, none of the above technologies has been developed and tested to a point where it can be scaled and accepted as a replacement for conventional mammography. However, greater focus and development in breast imaging could lead to a far more valuable outcome. The variance in breast imaging programs and guidelines for healthcare providers is vast. The most important step that must be taken in improving breast screening is to harmonize global standards. Screening and diagnosis pathways must become more adaptable to fit the individual being screened, and pathways must be developed using a multimodality approach, to best suit and diagnose each individual case.
So, what is the overall outlook for mammography screening in the future?
In the short term, little change can be expected. Rising healthcare costs and increasing red tape is limiting and slowing the development of new technologies and applications. Conventional mammography, one of the least expensive and most utilized screening techniques, will continue to be used, as it offers the widest access to the population for basic screening. Furthermore, the development of a full replacement for mammography is a long way off. Instead, new technology such as those mentioned above, must be implemented and used in a complementary fashion, increasing the accuracy of screening. Long term, ultrasound may be the final replacement. It's low cost, rapid advances in the last 10 years, and flexibility all point to strong potential for future screening capability.
Stephen Holloway is the lead analyst for medical imaging research at InMedica, and Carly Reed is a market analyst with the same company. InMedica publishes a range of market reports about the medical imaging industry. For more details, visit www.in-medica.com.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com or AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.