Diffusion-weighted imaging (DWI) is easy to acquire, has become a fine problem-solving tool in most circumstances, and is an important complement to other sequences in oncology imaging, attendees learned in Barcelona at the 2013 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) congress.
"In addition to characterizing benign from malignant lesions, DWI can be used in predicting and evaluating treatment response for rectal cancer," noted Dr. Arun Jacob, consultant radiologist at the University Hospital of North Staffordshire in Stoke-on-Trent, U.K. "DWI plays an important role in lesion characterization for evaluating metastatic disease. In this respect, DWI has proved to be equivalent to liver-specific postcontrast scanning, if not slightly better."
 It is difficult to confidently delineate the local invasion of this low rectal tumor on the axial T2-weighted image. The DWI fusion image not only outlines the tumor but also defines its invasion through the muscularis. All images courtesy of Dr. Arun Jacob and Dr. Muthukumarasamy Balasubramaniam.
It is difficult to confidently delineate the local invasion of this low rectal tumor on the axial T2-weighted image. The DWI fusion image not only outlines the tumor but also defines its invasion through the muscularis. All images courtesy of Dr. Arun Jacob and Dr. Muthukumarasamy Balasubramaniam.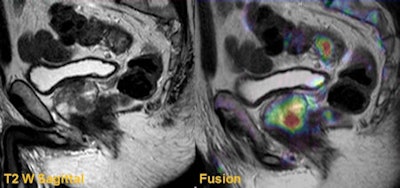 Sagittal T2-weighted and fusion images from a rectal staging examination show an upper rectal tumor. Fusion images also identified a clinically significant prostate cancer that had a significant impact in radiotherapy and treatment planning.
Sagittal T2-weighted and fusion images from a rectal staging examination show an upper rectal tumor. Fusion images also identified a clinically significant prostate cancer that had a significant impact in radiotherapy and treatment planning.It's vital to understand the additional value of DWI in rectal cancer imaging, given the technique's usefulness in tumor detection, tumor characterization, tumor staging, predicting and evaluating tumor response to preoperative chemoradiotherapy, tumor surveillance, and extracolonic findings, he added.
MRI is the modality of choice for local staging of rectal cancer, and it provides excellent anatomical detail of the rectal wall, mesorectal fascia, peritoneal reflection, and adjacent pelvic organs. For the local staging of rectal cancers, standard MRI sequences provide very good anatomical delineation, but it has limitations. Postbiopsy changes, post-treatment fibrosis, and benign background changes cause difficulty delineating the presence and extent of the tumor.
"DWI exploits the inherent diffusibility of water molecules at a microenvironmental level," Jacob stated in a recommended e-poster. "DWI offers significant advantages over conventional MRI in detection and management of rectal cancer."
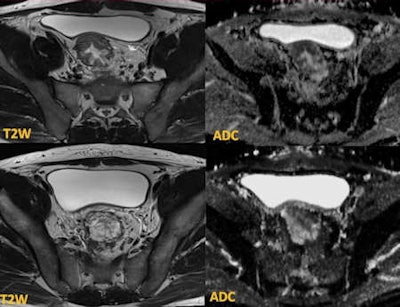 The initial biopsies showed tubulovillous adenoma with no invasion. MRI demonstrates tumor in the sigmoid (upper row) with restricted diffusion. The lower row of images at the rectosigmoid shows T2 high-signal lesion with T2 shine-through effect on the apparent diffusion coefficient (ADC) map -- tubulovillous adenoma. Targeted biopsies confirmed adenocarcinoma, and the patient required chemotherapy before surgery.
The initial biopsies showed tubulovillous adenoma with no invasion. MRI demonstrates tumor in the sigmoid (upper row) with restricted diffusion. The lower row of images at the rectosigmoid shows T2 high-signal lesion with T2 shine-through effect on the apparent diffusion coefficient (ADC) map -- tubulovillous adenoma. Targeted biopsies confirmed adenocarcinoma, and the patient required chemotherapy before surgery.The important prognostic factors in rectal cancer management -- such as depth of extramural invasion (T staging), presence of lymph node metastases, vascular invasion, and involvement of the circumferential resection margin -- can be accurately assessed on MRI. These factors dictate preoperative management through intense chemoradiotherapy. MRI is also very useful in staging locally advanced rectal tumor (T4 disease), such as the tumor invading the peritoneal reflection and adjacent pelvic organs. In addition, MRI is routinely used in assessing the tumor response to preoperative chemoradiotherapy.
Differentiating the tumor from the rectal wall often is difficult on fast spin-echo (FSE) T2-weighted (T2W) imaging, he continued. In particular, a small, low rectal tumor can be challenging because of the contrast difference between the tumor and adjacent intrinsic and extrinsic sphincter complex. In such circumstances, DWI with high B-values plays a major role in identifying the tumor. Coregistering high-resolution T2W images with the DWI and apparent diffusion coefficient (ADC) map significantly increases the sensitivity of identifying the tumor.
High-resolution T2W imaging demonstrates detailed anatomy of the rectal wall, but due to low contrast between the tumor and the rectal wall, accurate staging can be difficult, he confirmed. On the B-value images, although the signal-to-noise ratio is low, the contrast between the high signal tumor and the rectal wall can be clearly demonstrated. Moreover, when the DWI is coregistered with T2W images, the T-staging can be performed with high accuracy.
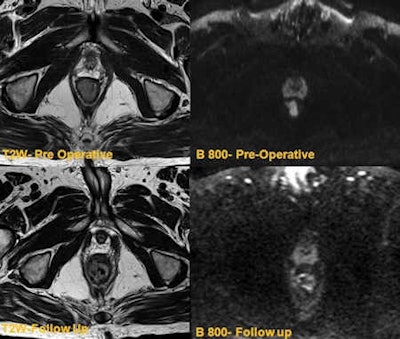 The top row shows low rectal tumor with restricted diffusion. The bottom row shows follow-up T2-weighted image demonstrating minor residual mucosal thickening. DWI shows no residual restricted diffusion, indicating post-treatment scarring.
The top row shows low rectal tumor with restricted diffusion. The bottom row shows follow-up T2-weighted image demonstrating minor residual mucosal thickening. DWI shows no residual restricted diffusion, indicating post-treatment scarring."Peri-tumor fibrosis, desmoplastic reaction, edema, inflammation occur following combined chemoradiotherapy. This poses a considerable diagnostic challenge in restaging because these post-treatment responses can produce spiculated margins and the signal characteristics resemble residual tumor on T2-weighted images. Hence overstaging is potential problem," wrote Jacob, whose co-author was Dr. Muthukumarasamy Balasubramaniam, a specialist registrar at the same institution. "DWI overcomes this pitfall as these changes do not demonstrate restricted diffusion, and the ADC values are generally high, proving to be a useful clinical tool."
Moreover, small residual tumors within the post-treatment changes can also be clearly demonstrated in DWI imaging as these tumors show high signal on high B-value due to restricted diffusion.
Patients who have responded well (complete responders) to initial chemoradiotherapy may be treated under a "wait and watch policy," and in this group of patients, DWI can be used for tumor surveillance, according to the authors. This is becoming an effective alternative for patients who do not want surgery or are not fit for a procedure. Early identification of local recurrence can be salvaged by minor endoscopic resection, avoiding major colorectal surgery.
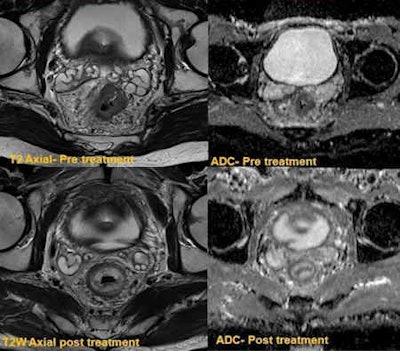 The top row shows circumferential tumor with significant restricted diffusion. The bottom row was obtained following downstaging chemoradiotherapy, which confirmed complete response. There is no residual tumor on postresection histology.
The top row shows circumferential tumor with significant restricted diffusion. The bottom row was obtained following downstaging chemoradiotherapy, which confirmed complete response. There is no residual tumor on postresection histology."There have been major recent advances in focal and endoscopic techniques, with procedures such as transanal resection of tumor (TART) and transanal endoscopic micro surgery (TEMS) now becoming an increasingly common first line of treatment. However there are substantial challenges in surveillance of these patients," they noted. "Post-treatment fibrosis can often be difficult to differentiate for residual tumor on endoscopy or standard MRI. DWI can be of considerable value in follow-up of this group of patients."
Patients with rectal cancer may have coexisting cancer of other pelvic organs such as the prostate and bladder. DWI can identify these tumors. Early detection of coexisting tumors is vital to ensure the best outcome for these patients because surgical and radiotherapy planning in these cases can be quite complex and often requires a multidisciplinary approach.
DWI also plays an important role in lesion characterization in focal liver or splenic lesion, Jacob and Balasubramaniam concluded. Identification of large metastatic deposits in conventional T2W turbo spin echo is straightforward, but small lesions (< 10 mm) can be difficult to identify because of difficulty in delineating small lesions from blood vessels. Respiratory movement artifacts can also significantly degrade both T2W and postcontrast images, making the lesion less conspicuous.