Dual x-ray absorptiometry (DEXA) is typically used to measure bone mineral density at the spine or hip to diagnose osteoporosis or evaluate treatment response. Certain conditions, however, alter bone density at other skeletal sites, leading to increased fracture risk that's not reflected by standard DEXA measurements.
U.K. researchers have now used a Hologic scanner to assess bone density at six lower limb sites. All measurements used the scanner's standard whole-body DEXA scan, which takes five minutes with a radiation dose of 4.2 µSv, and did not require any dedicated acquisition parameters or additional radiation dose (Physiological Measurement, July 2013, Vol. 34:7, pp. 757-768).
"Some patients, such as those with neurological dysfunction like stroke or spinal cord injury, experience bone loss at sites that are not commonly investigated by [DEXA] scans," explained Michael Haddaway from the Robert Jones and Agnes Hunt Orthopaedic Hospital NHS Foundation Trust in Oswestry. "This study was motivated by our experience with younger patients with spinal injury who often took part in physical wheelchair sports and who frequently suffered fractures around the knee, due to immobilization bone loss."
Subregion analysis
Haddaway and colleagues examined 30 subjects referred for DEXA scanning. Each patient underwent a whole-body DEXA scan, repeated after they got off and back onto the scanning couch to evaluate repositioning errors. This set of scans was used to undertake a lower limb analysis (LLA), using Hologic's existing subregional analysis software.
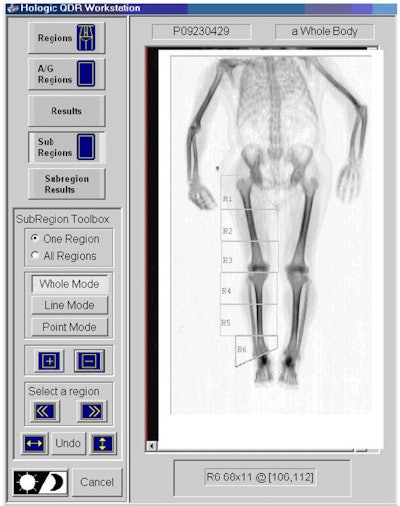 The six manually defined subregions (R1 to R6) within the lower right leg used to acquire subregional bone mineral density.
The six manually defined subregions (R1 to R6) within the lower right leg used to acquire subregional bone mineral density.This analysis program generates six regions (R1 to R6), covering each lower limb. The right femur and tibia were each subdivided into three regions (femur: R1 to R3; tibia: R4 to R6), of equal length where possible, with the lower margin of R3 and the upper margin of R4 passing through the knee joint space.
To determine system repeatability, the researchers calculated the coefficient of variation (CV) by comparing pairs of measurements separated by patient repositioning. Over all subjects, CV ranged from 1.7 to 4.5%, with the lowest values (indicating the greatest precision) seen at the mid (R2) and lower (R3) femur. The highest values were seen close to the hip (R1) and the ankle (R6), sites that are most subject to variation in patient position and also those used for fine adjustments within the protocol.
The CV for R5 (midtibia) of 4.2 was unexpectedly high. The authors propose that this is due to the relative contribution of cortical and trabecular bone varying between patients at this site. They note that CV values for R2 to R4 compared well with the precision seen for conventional DEXA hip and spine measurements.
The researchers also derived the least significant change (LSC), the value representing the smallest change in bone density that is clinically significant. Calculated LSC values were 9.8%, 4.6%, 7.1%, 7.2%, 11.5%, and 12.4%, for R1 to R6, respectively. "Once a change exceeds an LSC value, then it may be considered more than just a statistical change and may therefore be biologically meaningful," Haddaway explained. "Hence, LSC values help with making clinical decisions."
Operator variations
Finally, the team examined inter- and intraoperator variations in 10 subjects, with three operators analyzing each measurement three times. Intraoperator CV, a measure of an individual operator's precision at repeating the same analysis, was calculated from three measurements on 10 subjects. Intraoperator precision was between 1.0% and 2.9%, with no significant difference seen among operators.
Interoperator variability, calculated for the first and third sets of results obtained by each operator, was between 1.0% and 3.6%, according to region. This indicates that the individual operators are achieving good precision with this protocol and also that agreement among operators is robust. Comparing the first and the third measurements revealed no evidence of a learning effect with repeated analyses.
While this study looked specifically at bone mineral density in regions of the lower limb, the technique is equally applicable to the upper limbs, Haddaway noted. It could also be used to study body composition (bone mineral, muscle, and fat content) in the arms and legs.
"Although developed for use in spinal injury patients who undergo rapid changes in the tissues of the lower limb, the method has broad clinical potential and could be applied to many types of patient," Haddaway said. "This includes those with muscular dystrophy, multiple sclerosis, or stroke, to follow the extent of bone and tissue loss in the limbs and also to follow the efficacy of therapeutic and rehabilitation regimes."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.