A new technique aimed at mapping CT radiation dose individually for each patient is showing just how far from reality the current standard for calculating dose can be, especially in obese patients, researchers concluded at the 2013 European Congress of Radiology (ECR).
Currently, CT dose is calculated with conventional dose-length product (DLP) conversion (k) factors, which are based on standardized phantoms. But real patients rarely correspond to standard phantom sizes, which leads to disparities between the actual doses they receive in CT scans and dose estimates based on the DLP method.
"We don't do a good job with our currently available dose-estimation techniques of representing patients' exposure on the basis of size," lead study author Sandra Halliburton, PhD, from the Cleveland Clinic, told AuntMinnie.com. "Patient size matters with respect to absorbed dose," she said.
Instead of using the DLP method, the researchers based their dose estimates on individualized dose maps that used the patients themselves as "phantoms" derived from their CT data. The group found that estimates varied by as much as one-third between totals calculated using conventional DLP conversion (k) factors and the new patient dose-mapping technique; in addition, the dose differences between the methods increased with increasing patient size, according to investigators from the Cleveland Clinic, the University of Cleveland, and Philips Healthcare, which supported the study.
Once perfected, the dose-estimation scheme could improve CT dose estimates considerably, the research team concluded.
"Patient dose derived from patient mapping is more accurate because it takes into consideration the patient size as well as the individual organs," said Carla Thompson in the ECR talk. Thompson is a doctoral student in the applied biomedical engineering program at Cleveland State University and the Cleveland Clinic Foundation.
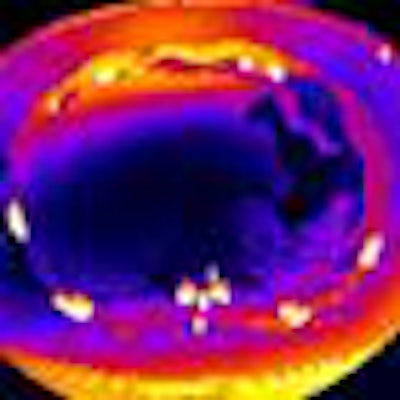
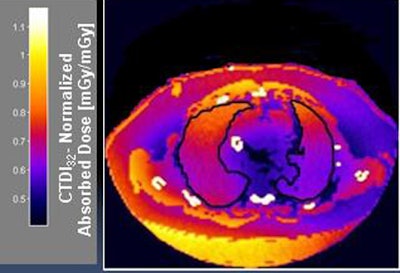 Individualized dose maps account for patient size and individual organ dose. All images courtesy of Carla Thompson and Sandra Halliburton, PhD.
Individualized dose maps account for patient size and individual organ dose. All images courtesy of Carla Thompson and Sandra Halliburton, PhD.Effective dose (ED) is a dose descriptor that reflects the biological sensitivity of irradiated organs and tissues, Thompson explained. ED levels are typically calculated for CT scans using Monte Carlo simulations based on a 70-kg adult reference phantom with standard fixed organ sizes. In clinical practice, effective dose is estimated as DLP multiplied by a "k" conversion factor, and DLP is the absorbed dose along the scan length based on measurements performed on a 32 x 16-cm Plexiglas phantom.
The study aimed to compare effective doses derived from the two methods in 15 patients (mean age, 51 years; seven women and eight men), who had a mean body mass index (BMI) of 35 (range, 26-45 kg/m2). Five were referred for coronary artery evaluation, five for pulmonary vein evaluation, and five for thoracic aorta evaluation. Cardiac CT datasets were acquired on a 256-detector-row scanner (iCT, Philips), using nongated helical retrospective electrocardiogram (ECG)-gated or prospective ECG-triggered axial techniques.
Image reconstruction of the full field-of-view was performed for the coronary arteries, pulmonary veins, or thoracic aorta with scan lengths ranging from 120 mm to 600 mm. The datasets were processed offline with a prototype Monte Carlo simulation tool (Philips) that enabled the adjustment of both tube potential and tube current-time product, utilized original scan parameters, and modeled scanner geometry including the tube start angle.
Each dataset was then "voxelized" to create a patient-specific virtual phantom. Each voxel was assigned a material type based on a priori global HU classification intervals per the International Commission on Radiation Units and Measurements Report 44.
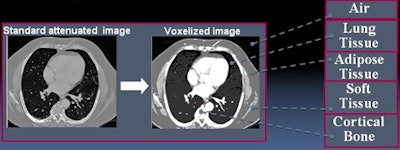 Each voxel in the voxelized datasets was assigned a specific material type based on International Commission on Radiation Units and Measurements Report 44.
Each voxel in the voxelized datasets was assigned a specific material type based on International Commission on Radiation Units and Measurements Report 44.
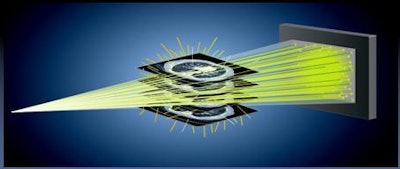 Monte Carlo simulation was applied to voxelized image sets (prototype simulation tool, Philips).
Monte Carlo simulation was applied to voxelized image sets (prototype simulation tool, Philips).Two readers manually segmented skin, lungs, breast, stomach, liver, and esophagus regions from dose maps, then determined the effective dose.
"Our method is more patient-specific because we're not only including the patient dataset, we also calculate the individual organ dose from each map, and then multiply that by the tissue weighting factor to come up with the effective dose," Thompson said.
The method bases average effective dose on the weighted sum of organ doses from the International Commission on Radiological Protection (ICRP) Publication 60. The "ED = k chest x DLP" formula was compared with a two-tailed paired Student's t-test. The group then computed the mean of absolute percentage differences between the two ED estimates. ED dose map/ED k-factor ratios and BMI were plotted in Cartesian coordinates. One patient was removed from the analysis due to a portion of the anatomy being outside the scan field, leaving 14 patients.
According to the results, the average effective dose was not significantly different between the dose-mapping and DLP methods (4.7 mSv for dose mapping versus 4.3 mSv, p = 0.76), the group reported.
The results were somewhat different for obese patients, however. Effective dose ratios compared to BMI showed a trend toward overestimation of dose by the k-factor method relative to the dose-map method.
"In obese patients, we are actually overestimating the risk with our standard, admittedly very crude method of multiplying DLP by a k factor," Halliburton said.
Results in nine obese patients showed significant differences between dose-map and DLP calculations. The average effective dose measured with the dose-map method for the nine patients was 4.9 mSv, compared with an average of 6.4 mSv with the DLP method (p < 0.05).
"For patients with BMI of 30 and up, we noticed a significant difference shown by paired t-test, and we saw that the effective dose [map] method was lower, with an average of 4.9 mSv as compared to the standard method of 6.4 mSv," she said. "This makes sense because we can see that the DLP doesn't account for patients that deviate from the 32-cm Plexiglas phantom -- it's obvious here that the standard method is going to overestimate the dose for obese patients."
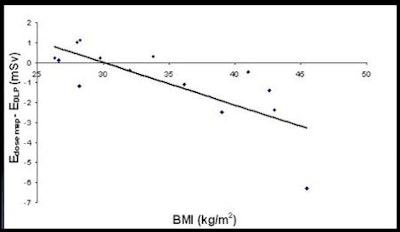 For obese patients, the difference in the effective dose estimates increases with patient size (BMI). There was a significant difference found between the two effective dose methods based on a nonzero intercept from the least squared regression analysis controlled for BMI (p < 0.05).
For obese patients, the difference in the effective dose estimates increases with patient size (BMI). There was a significant difference found between the two effective dose methods based on a nonzero intercept from the least squared regression analysis controlled for BMI (p < 0.05)."All the tissue that an obese patient has surrounding the heart acts as a bit of an insulator," Halliburton said. "That fat is not particularly radiosensitive, and it's absorbing a lot of the x-ray beam."
Breast tissue is a different matter, she said. If the same x-ray parameters are used on two individuals, an average-weight person and an obese person, the thinner person would be at greater risk because they're absorbing x-rays in their more radiosensitive organs; the larger person is going to absorb x-rays in less radiosensitive organs.
The research team concluded that dose estimation differences increased with patient size, and that the dose-map method provided lower estimates of effective dose compared to the DLP method. The lower dose is likely more accurate, especially in these patients, because dose maps account for differences in patient size as well as individual organ size, Thompson said. Patient-specific dose maps could improve CT dose estimation, potentially improving CT dose management, she added.
When asked how long it took to process each map, Thompson said the technique is not ready for clinical use because with all the calculations it takes several hours to produce one patient map. But it offers a better representation of dose, and with time it may become more patient-specific, she said.
"The reason I got involved with this was the hope that maybe, eventually, information could be used in a feedback loop mechanism if it was available soon enough," she said. "You could make a decision based on a patient's particular body type and tissue distribution; you could perhaps make a decision about which dose-reduction techniques might be most effective in a given patient."



















