Computer-aided detection (CAD) technology can yield high sensitivity, albeit with low specificity, for finding very small invasive breast cancers on full-field digital mammography (FFDM) studies, Spanish researchers have found.
In a retrospective study involving 68 invasive cancers ≤ 1 cm in size, a team led by Dr. Xavier Bargalló of Hospital Clínic de Barcelona in Spain found that CAD produced overall sensitivity of 86.7%. However, per-study specificity was only 26%.
"CAD shows a high sensitivity and a low specificity in detecting very small invasive breast cancers from our population-based screening program," the authors wrote.
The research team shared their findings in an article published online in the Journal of Digital Imaging (November 7, 2012).
While the reported sensitivity of CAD in FFDM studies has varied in prior research from 78% to 96%, none of these studies focused on very small, invasive breast cancers detected at screening, according to the authors. As a result, the team sought to investigate CAD's performance in a study that included 68 invasive breast cancers ≤ 1 cm in size from women aged 49 to 69 in their population-based breast screening program in three districts of Barcelona.
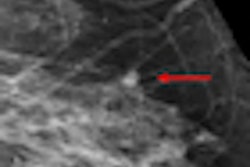
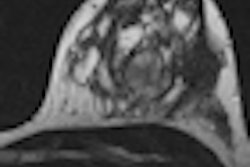
They also wanted to assess the mammographic features of the lesion, breast density, size, and histology to determine their influence on CAD. Version 7.2 of SecondLook CAD software (iCAD) was applied to the FFDM images, which were acquired using a Senographe 2000 D system (GE Healthcare). All cases included craniocaudal (CC) and mediolateral (MLO) views of the breast with cancer at time of diagnosis.
Two radiologists with subspecialization in breast imaging recorded the mammographic patterns of all visible cancers and classified lesion types as: masses, calcifications, masses with calcifications, architectural distortions, and asymmetries. Masses were classified by morphology, margins, and density, while calcifications were classified according to their morphology, the number of flecks per cluster, and the size of the cluster.
Each lesion was also retrospectively assigned a final BI-RADS category. In accordance with European guidelines, double reading of each screening mammogram was performed with arbitration of discordant readings.
After CAD processed the raw image data, it sent them to the PACS. CAD marks on these images were then checked on PACS and classified as either true-positive or false-positive.
Of the 68 cancers, 37 (54.4%) were masses, 17 (25%) were calcifications, six (8.8%) were masses with calcifications, seven (10.3%) were architectural distortions, and one was an asymmetry (1.5%).
Overall, CAD detected the invasive cancer in 59 (86.7%) of 68 cases.
CAD sensitivity by mammographic appearance of cancer
|
Of the nine that were missed, five were masses, three were architectural distortions, and one was an asymmetry.
In further analysis of the data, the group discovered that lesion size (between 1 and 10 mm), histology, and breast density do not influence CAD sensitivity, but mammographic features were an important factor.
"Thus, all invasive cancers showing calcifications and all hyperdense masses were correctly prompted," they wrote. "Lesions assigned as BI-RADS 4c-5 and thick spicules in architectural distortions seem to be easier to detect by CAD."
As has often been the case with CAD, the technology suffered from low specificity (26%). The false-positive rate was 1.76 marks per mammography study.
The radiologist readers had 14 false-negative readings, including six masses, four calcifications, three masses with calcifications, and one architectural distortion. CAD, however, correctly marked 11 of these, missing only two masses and the architectural distortion.
The study results show that CAD performs well for detecting high-density masses and calcifications but fails to find some isodense masses and very thin spicules, the researchers noted.
"Moreover, the number of false-negative marks can be distracting for the radiologist," the authors wrote. "We think that future developments of this technology should attempt to correct these limitations."