Acute stroke patients should be evaluated by noncontrast CT followed by perfusion CT, while MRI should be reserved for more chronic cases of brain ischemia or control examinations in stroke patients. That's the recommendation of an experienced group of specialists from the Czech Republic.
When state-of-the-art CT and high-quality MR scanners are used, however, both techniques are practically equivalent in the hands of experienced staff, and local clinical configurations may often dictate which technique should be used, noted lead author Dr. Josef Vymazal, PhD, a professor in the department of radiology at Na Homolce Hospital in Prague.
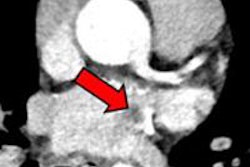
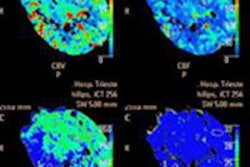
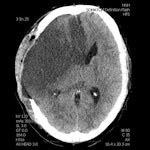 A 28-year-old male with a history of aortic valve replacement and poor compliance with anticoagulative medication, presented with sudden left-sided hemiplegia. No penumbra was apparent on perfusion CT, as shown in left figure (CBF) and middle figure (CBV). Standard CT image (right figure) two days following decompressive craniectomy shows significant mass effect with dislocation of midline structures. Images courtesy of Dr. Josef Vymazel.
A 28-year-old male with a history of aortic valve replacement and poor compliance with anticoagulative medication, presented with sudden left-sided hemiplegia. No penumbra was apparent on perfusion CT, as shown in left figure (CBF) and middle figure (CBV). Standard CT image (right figure) two days following decompressive craniectomy shows significant mass effect with dislocation of midline structures. Images courtesy of Dr. Josef Vymazel.When ultrafast CT scanners covering almost the entire brain are used, the potential to detect ischemia and salvageable tissue is very similar to MRI. However, the major drawback of CT is the high radiation dose, while in MRI it is the more complicated and time-consuming aspect of the examination, he wrote in an article published online on 29 September by Insights into Imaging.
"The introduction of perfusion CT (PCT) of the brain has significantly improved the sensitivity and specificity in detecting fresh ischemia. Perfusion deficit can be detected immediately after stroke, i.e., in the time when a standard CT is still negative," Vymazal stated.
A major drawback is the limited coverage of the brain with older CT scanners, and in such cases the coverage is limited to several slices and the neurologist or neuroradiologist has to decide which part of the brain should be covered. Misleading neurological symptomatology may lead the physician to set the perfusion slab in the wrong position, so 75-mm brain coverage is the minimal PCT coverage recommended in selecting patients with acute stroke for reperfusion therapy, he explained.
Ultrafast CT scanners together with iterative reconstructions can significantly reduce the radiation dose, but in PCT of the brain the dose still remains relatively high (mean effective dose is approximately 5 mSv). The long reconstruction times of iterative techniques are inconvenient for stroke patient management, but there are techniques that can decrease the radiation dose to values comparable to unenhanced brain CT (approximately 2 mSv), according to Vymazal and colleagues.
"A decrease from 140-120 kV to 100-80 kV not only significantly lowers the radiation dose, but also increases the prominence of the contrast agent because of the greater importance of the photoelectric effect for 80-kV photons," they wrote. "Another method for dose reduction relies on decreasing the image frequency of acquisition from the PCT first-pass data. PCT enjoys a number of advantages as it is fast, widely available, and cost-effective. Furthermore, there are few restrictions in the CT environment."
A number of pitfalls must be considered in performing PCT. The operator-dependent selection for the arterial input function may have a substantial impact on results, especially in patients with chronic vascular conditions such as giant aneurysm or carotid artery occlusion, as well as in those with asymmetric microvascular changes. Postictal changes are another concern; lateralized postictal hyperperfusion may lead to the erroneous diagnosis of contralateral ischemia on visual inspection of color maps, they warned. Additionally, postprocessing and modeling methods may affect the results and complicate comparison across studies.
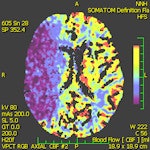
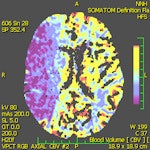
Different parameters are used in routine clinical practice for the detection of penumbra with CT and MRI. The subtraction of cerebral blood flow (CBF) and cerebral blood volume (CBV) is the usual way to detect penumbra using CT, according to the authors. On MRI, a subtraction between perfusion parameters (mean transit time, time to peak, or CBF) and diffusion-weighted imaging, rather than CBV, is used because CBV (especially on MRI) is not sensitive enough to detect small lesions. Such lesions are easily detected with DWI, according to the authors. DWI, on the other hand, may underestimate the final stroke volume and grows into CBV over the time.
"The penumbra concept is far from straightforward, however, as a number of different factors determine whether the tissue will become necrotic, such as the time-dependent nature of morphological changes discussed previously," the authors wrote. "The situation is even more complicated because exact quantification of perfusion values (CBF, CBV) is rarely used in routine clinical practice. Thus, relying only on CBF/CBV mismatch might disqualify some patients that would benefit from intervention."
Even in critically hypoperfused tissue, only a part of the predicted final infarct volume became necrotic after thrombolytic therapy, they noted. For these reasons, no quantitative parameters related to the penumbra should be taken for granted, and neuroimaging of the penumbra based on the presence of mismatch on CT or MRI may bring ambiguous results in relation to treatment outcome.