Computer-aided detection (CAD) systems should not replace radiologists or be used for final interpretation, despite its growing use as a second reader to reduce the number of false-negative mammograms, researchers from the Paris region have advocated in the European Journal of Radiology.
CAD has become increasingly popular. It helps catch what the radiologist may have missed on the mammogram because he or she was distracted or there is complex breast architecture. The most frequent reason for missed breast cancers is the misinterpretation of a perceived abnormality, which is slightly more common than overlooked cases, according to Dr. Clarisse Dromain from the radiology department at Institut Gustave-Roussy in Villejuif, France.
The aim of the CAD system is to offer more objective evidence and increase the radiologist's diagnostic confidence, noted Dromain and colleagues, who reviewed mammography CAD systems and their performance in assisting reading screening mammograms, as well as MRI CAD and ultrasound CAD systems (European Journal of Radiology, 29 August, article in press).
"CAD systems are image analysis tools intended to reduce the number of false-negative mammograms that can be caused by subtle findings, radiologist distraction, or complex architecture," she wrote. "The use of a CAD system helps the radiologist as a second reviewer to evaluate screening mammograms. However, CAD must not be responsible for omitting the step of the complete evaluation of mammograms by the radiologist. A CAD system cannot and should not replace the radiologist as either or final interpretation."
CAD in mammography
CAD-assisted reading is associated with a moderate increase in sensitivity and with a drop in specificity, according to several published studies. In one, by Freer et al (Radiology, September 2001, Vol. 220, pp.781-786), among 12,860 mammograms, there were 986 recalls and 49 cancers. Eight of the cancers were detected with CAD alone, which increased the detection rate by 19.5%.
In a more recent study published in the New England Journal of Medicine, the researchers concluded the use of CAD is associated with reduced accuracy of screening mammogram interpretation, an increased rate of biopsies, and is not clearly associated with enhanced detection of invasive breast cancer (NEJM, April 2007, Vol. 356:14, pp. 1399-1409). CAD increased sensitivity from 80.4% to 84%, decreased specificity from 90.2% to 87.2%, and increased the rate of biopsies by 19.7%, and the rate of detection of invasive cancer decreased by 12%.
CAD certainly has its uses and thus is well-situated for use as a second reader. "[I]t is well established that prospective double reading of screening mammograms increases the detection of cancer from 4% to 15%, Dromain wrote. "Like double reading, CAD could increase the cancer detection rate and could be easier to implement and cheaper than double reading."
Several studies back this up, including one by Gilbert et al, showing single reading with CAD yielded the same performance as double reading (NEJM, October 2008, Vol. 359:16, pp. 1675-1684). The proportion of cancers detected was 87.7% for double reading and 87.2% for single reading with computer-aided detection. However, the specificity of CAD is low with about one false positive mark per view. These false positive marks may cause the radiologist to underestimate and disregard CAD findings.
CAD's performance
"The performance of CAD in breast cancer detection is dependent on the performance of the CAD itself, the population to which it is applied, and on the radiologists who use it," according to Dromain. "Most studies suggest that there is a clear benefit in using CAD in less experienced or low-volume reviewers." In one such study, the use of CAD improved sensitivity from 61.9% to 84.6% in junior radiologists and 76.9% to 84.6% for experienced radiologists.
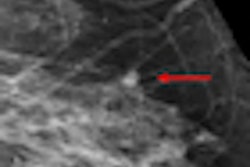
CAD devices are particularly helpful in detecting breast carcinomas presenting as microcalcifications, with a reported sensitivity for microcalcification detection ranging from 86% to 99%, she added.
"CAD clearly increases the efficiency and confidence level of radiologists when searching for subtle microcalcifications," she wrote. "Moreover, the rate of false-positive marks is about 0.6 marks/image and is lower than for mass detection."
The performance of CAD may also depend on background breast density and histologic findings in the tumor. Other studies suggest CAD could have a greater sensitivity for detecting invasive lobular carcinoma and ductal carcinoma in situ rather than for invasive ductal carcinoma.
CAD in breast MRI
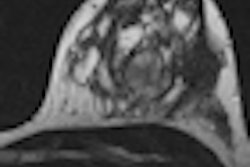
MRI has a particular high rate of sensitivity in screening for breast lesions (78-98%) but its specificity is still lacking (43-75%). "These last years have seen the development of computed-assisted diagnosis software in order to facilitate the MR analysis and the report, or to try to improve the characterization of MR-detected lesions," Dromain wrote.
The software systems analyze dynamic contrast-enhanced breast MRI and generate parametric maps with a detailed evaluation of the uptake kinetics of the contrast agent in enhancing lesions. Most of the commercially available systems exclusively analyze kinetic studies, without analyzing morphological parameters.
Lehman et al evaluated one such software (Cadstream, Confirma) in 33 suspicious lesions that were detected on MRI and biopsied under MR guidance. All malignant lesions showed significant enhancement and were correctly identified by the software, with a sensitivity of 100% (American Journal of Roentgenology, July 2006, Vol. 187:1, pp. 51-56). The false positive rates for the CAD software compared to the radiologist's analysis were reduced by 25% at a 50% threshold, by 33% at an 80% threshold, and 50% at a 100% threshold for enhancement.
In Lehman's study, the CAD MR software showed a high accuracy with improved specificity without decreasing sensitivity. The results were confirmed in a recent study, comparing three commercially available CAD MR systems: Cadstream (Confirma), 3TP Server Version 2.2.4 (CADsciences), and Mammatool (Digital Image Solutions). MRI studies of 21 patients were analyzed with all three software programs. All 10 carcinomas were considered as malignant lesions by the three CAD softwares. In addition, 131 further benign lesions were marked in Cadstream, 133 in 3TP, and 99 in Mammatool, which had the lowest false-positive rate (EJR, February 2009, Vol. 69:2, pp. 300-307).
CAD in ultrasound
The first commercially developed software for ultrasound is B-CAD from Medipattern. Other "homemade" systems have also been developed by working teams in imaging research but the general physics principles are usually the same.
In B-CAD, the radiologist places a mark in the center of the nodule on the screen, and the system automatically draws the contours of the lesion to extract the different morphological parameters. The drawing may be inaccurate, but the radiologist can manually readjust the margins to achieve adequacy. The CAD system analyzes the extracted parameters and proposes an evaluation.
In most of the studies, the use of dedicated CAD software for breast ultrasound improves the accuracy in classifying benign and malignant breast lesions but the performance of CAD can vary according to the type of lesion (benign or malignant, cystic or solid), Dromain wrote. In a recent study, 1,046 lesions on 2,266 images were analyzed by an ultrasound CAD system. Sensitivity was 100% and specificity was only 30% -- the expected specificity of the radiologist was 77% (Radiol, August 2008, Vol. 248:2, pp. 392-397).
"A literature analysis of ultrasound CAD accuracy is ambiguous: some studies show the poor specificity of the different systems, while other authors underline the great value of CAD in terms of specificity, allowing a decrease of up to 53% in the need for biopsy," she stated. "The performances of CAD systems are usually better in the case of suspicious lesions, with a high risk of malignancy compared to benign lesions. Usually the cystic lesions are the least difficult to deal with using a CAD system, whereas the other benign solid lesions are more difficult to analyze."
In addition, specificity is often lower in the case of benign nodules but nevertheless, an ultrasound CAD system can be used as a teaching tool for junior radiologists, especially to familiarize them with the different terms of the breast ultrasound BI-RADS lexicon, Dromain wrote.