Heart and whole-body MRI is a feasible technique with demonstrated accuracy in detecting atherosclerotic disease. Still, screening consecutive, presumably healthy patients for signs of cardiovascular disease with whole-body MR, as German investigators did for a new study in Insights into Imaging, is rare enough to raise eyebrows.
The experiment was successful. About one-fourth of the cohort of 138 individuals -- mostly middle-aged males with various risk factors for atherosclerosis -- had vascular abnormalities. One-third required some kind of follow-up. As for the imaging exam itself, cardiac MR (CMR) was able to evaluate nearly 100% of the more than 2,000 vessel segments analyzed, wrote the researchers from University Hospital Munich in Germany.
"Whole-body MRI/MR angiography (MRA) is a safe, reproducible technique with few side effects," Dr. Mona Laible and colleagues concluded. Findings in the cohort "led to an application of additional diagnostic measures or intensified control intervals in our study subjects" -- which in many cases meant giving patients lipid-lowering medications alone, they explained. "Therefore, in combination with the modification of cardiovascular risk factors, possibly fatal cardiovascular events might be prevented," the study team wrote (Insights into Imaging, 26 July 2012).
Not every modality is adequate for assessing the presence of atherosclerosis in asymptomatic individuals, but MRA is a good candidate owing to its lack of ionizing radiation, noninvasive nature, and lower toxicity vis-à-vis CT angiography (CTA) with iodinated contrast. And previous studies have shown that MRA has high sensitivity and specificity for gauging the extent of atherosclerosis in patients with vascular disease compared with digital subtraction angiography as the gold standard.
To date, however, whole-body MRA has mostly been confined to cancer staging and follow-up in individuals with a history of cancer, and not for vascular screening purposes. "Therefore, the primary intent of this study was not to determine the diagnostic accuracy of [whole-body] MRA, but to describe whole-body MRI findings in terms of atherosclerotic changes in a cohort of asymptomatic middle-aged individuals in Germany in an observational prospective study," Laible and colleagues wrote.
The study examined 138 individuals (118 men, 20 women; mean age 54 ±7.55 years) who were referred for whole-body MRI at 1.5 tesla, including contrast-enhanced whole-body MRA and CMR.
Subjects with a history or symptoms of cardiovascular disease were excluded from the start, so although there were no symptoms, there were risk factors. The investigators recorded information about family history, smoking, lack of exercise, etc. Each participant also underwent a basic health exam that included an ECG at rest and stress, a blood panel, stress test using an ergometer, and imaging tests, including chest x-ray, transthoracic echocardiography, and duplex ultrasound of the carotid arteries.
MRA findings were classified as relevant (leading to further diagnostic workup) or nonrelevant (such as a renal cyst that requires no further intervention). The results of relevant control exams, when available, were compared case by case.
Scan protocols
The exams were conducted on one of two 1.5-tesla MRI systems: Magnetom Sonata (first 36 subjects) or Magnetom Avanto (last 102 subjects) both from Siemens Healthcare. The systems were equipped with multiple receiver channels and multielement surface coils enabling the use of parallel imaging techniques.
All subjects underwent whole-body MRI, beginning with noncontrast-enhanced MR of the lungs first using half-Fourier rapid acquisition relaxation-enhanced (RARE) techniques. Cardiac function imaging was then performed using high-resolution contrast-enhanced MRA.
Cardiac function was assessed using a real-time cardiac imaging sequence (true fast imaging with steady state-precession [true FISP]), acquired in two heartbeats for imaging a single slice of the heart. Cardiodynamic parameters including end-diastolic volume (EDV), end-systolic volume (ESV), ejection fraction (EF), and myocardial mass (MM), calculated using a modified Simpson's rule.
First-pass perfusion imaging of the heart at rest was performed using a saturation-recovery true FISP sequence, which used parallel imaging to acquire four slices in a single breath-hold, the authors wrote. Patients were injected with a gadolinium-based contrast agent at 0.05 mmol/kg body weight. Helpful as it might have been, stress imaging was not part of the exam as it is not ethically feasible in asymptomatic patients, the group noted. However, cardiac delayed contrast-enhanced imaging was acquired to exhibit any delayed hyperenhancment in the infracted myocardium. A phase-sensitive inversion-recovery sequence was used to enable delayed contrast-enhanced imaging without prior scout imaging, following a delay of 15 to 17 minutes.
Contrast-enhanced MR angiography was performed using parallel techniques for spatial resolution less than 1.5 mm3 for classification of mild stenosis (≤ 50% luminal narrowing), moderate stenosis (50% to 70%), or high-grade stenosis (≥ 70%). Two highly experienced radiologists evaluated the data individually, discussing and recording their findings in consensus.
Further tests in one-third
The results showed that all 138 participants successfully completed the whole-body MRA exam, and there were no adverse events. In 31% of participants, imaging findings led to further exams or intervention -- for example, beginning to take preventive medication.
A total of 26.8% of participants showed pathological changes in at least one vessel segment. Atherosclerosis was found in 18 (7.2%) of patients, and atherosclerotic changes were found in one vascular territory in 39 subjects. An additional 25 subjects (18.1%) had stenosis in a second arterial segment, and as many as five arterial vascular regions were affected in two cases (1.4%).
Fully 7.2% of the subjects showed mild to moderate luminal narrowing in at least one vascular territory, and another 5.8% had at least one stenosis of 50% or more. Meanwhile, 86.9% of individuals presented without any stenoses.
In the carotid arteries, stenoses were detected in seven individuals (4.9%), including four mild and two moderate cases. In one case, the researchers found a high-grade stenosis of the proximal carotid artery.
Aortic plaques were found in six cases, while iliac artery plaques were seen in four cases that lacked luminal narrowing. In all, there were 10 mild stenoses, seven medium-graded stenoses, and seven high-grade stenoses within the large arterial vessels, as well as two low-grade aortic aneurysms. In the kidneys, the group found one mild stenosis and one case of plaque without luminal narrowing.
The most commonly detected atherosclerotic abnormalities were in the lower leg, with 12 individuals presenting with mild (n = 2), moderate (n = 3), or severe (n = 7) stenosis.
Cardiac MR imaging found four cases of myocardial hypertrophy and also wall motion abnormalities in six individuals (4.3%). There was subendocardial delayed contrast enhancement in two cases and a perfusion deficit in 13 cases (9.1%). In nine men, there was global myocardial dysfunction with an ejection fraction of less than 50%.
Nine subjects had valve disease detected in the functional evaluation of the left ventricular myocardium, and two had findings consistent with aortic valve insufficiency, two had aortic stenosis, and two had mitral valve insufficiency, the authors wrote. There was one case with signs of pericarditis.
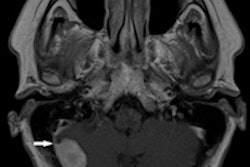
Incidental findings included five cases of pathologically enlarged lymphatic nodules, four inflammatory nodules, and one inflammatory infiltrate. Cerebral microangiopathy was seen in three cases, and white-matter lesions were present in an additional nine cases. There was one mengioma, but no malignant lesions detected in whole-body MRI.
High disease prevalence in asymptomatics
"This study showed that [whole-body] MRI can be performed and evaluated with the use of 1.5-tesla clinical MR systems," Laible and colleagues wrote. The feasibility of whole-body cardiovascular MRI has been shown in previous studies, but very few examined cohorts of healthy individuals, they noted.
"Our study provides useful information about the prevalence of cardiovascular disease in a large, relatively homogenous collective," they wrote. "Therefore, it contributes data to assess the significance of [whole-body] MRI/MRA in broad clinical use as a diagnostic screening tool." The finding of vascular pathology in more than 26% of subjects may support the secondary preventive use of the exam in a preselected population. However, long-term outcomes are unknown, and additional studies will be required to evaluate outcomes as well as cost-effectiveness, they wrote.
Previously, Hansen et al examined a cohort that was a mean 14 years older and found one-third of subjects with a luminal narrowing of greater than 50%, compared with 37% in the present cohort, which also included more males. Functional cardiac analysis in the current study found wall motion abnormalities in 3.6% of all study participants, and cardiac perfusion deficits in 8.7%, a little higher than other studies for patients without suspected heart disease. Generally, however, the prevalence rates for the presence of atherosclerosis and its complications were comparable to data from large epidemiological studies of middle-aged subjects, Laible and colleagues wrote.
It's useful to avoid the use of ionizing radiation in a cohort of apparently healthy individuals; however, ultrasound of arterial vessels rather than MRI might be a suitable alternative in some easily accessible anatomic regions, they wrote, adding that ultrasound has its own well-known limitations relating to operator dependence and confinement to a few vessels. Moreover, MRI is not the method of choice to evaluate vessel wall changes such as discriminating between hard and soft plaques, the group wrote. Also of note, no prospective studies have shown the benefit of intervention based on whole-body MRA findings -- so outcomes studies will be needed for whole-body MRI to become widely accepted.
"[Whole-body] MRI and ... MRA comprise a reliable, reproducible, and easily applicable diagnostic tool for the detection of atherosclerotic disease in all major arterial territories," Laible's team concluded. On the other hand, they added, the chance of finding a previously undetected malignancy in the same exam is low, making it unlikely that whole-body MRI will often succeed in doing double duty.