Whole-body MRI can detect vascular changes in patients with diabetes that can signal an increased risk of heart attack and stroke, according to a new study by German researchers published online September 10 in Radiology.
Researchers from Ludwig Maximilians University in Munich found that patients with detectable vascular changes on whole-body MRI faced a 20% chance of a major adverse cardiac and cerebrovascular event (MACCE) in three years. The chance increased to 35% for six years.
In addition, no patients in the study with normal whole-body MRI results experienced such an adverse event (Radiology, September 10, 2013).
"Patients without any pathologic findings on whole-body MR experienced no adverse events over the six-year follow-up period," lead author Dr. Fabian Bamberg, from the university's department of radiology, wrote in an email to AuntMinnie.com. "This is specifically interesting as the population had on average 10 years of diabetes."
Patients with good whole-body MRI results "may be reassured and encouraged that their therapeutic regimen is optimal," Bamberg added. "Conversely, the event rate among diabetics with pathologic findings was surprisingly high, indicating that more intensified treatment may be required."
Complications of diabetes
Individuals afflicted with diabetes often develop atherosclerosis, which results in a greater chance of heart attack and stroke, the authors wrote. Recently, MR has shown promise for cardiac imaging of diabetic patients, and whole-body MRI may be useful due to the systemic nature of the disease, according to Bamberg and colleagues.
"Due to its nonionizing nature, MR is the ideal imaging modality to perform whole-body acquisitions in this clinical setting," Bamberg said. "This is in contrast to more focused imaging techniques, such as coronary calcium scanning by CT or myocardial perfusion imaging, which are well-established modalities for risk assessment in diabetic patients."
In the current study, the researchers enrolled 65 patients with type 1 or type 2 diabetes and a disease duration of at least 10 years. The patients underwent contrast-enhanced whole-body MRI exams, including brain, cardiac, and vascular sequences at baseline, between June 2005 and December 2006. Imaging was performed on either a 3- or 1.5-tesla system (Magnetom Tim Trio or Magnetom Avanto, Siemens Healthcare).
Follow-up was conducted during July 2011 and May 2012 by phone interviews, evaluating medical records, or through a patient's physician to identify any major adverse cardiac and cerebrovascular events. These included cardiac and cerebrovascular death, nonfatal myocardial infarction, coronary revascularization, cerebrovascular disease, and/or carotid revascularization.
Four patients were lost to follow-up, leaving 61 in the final analysis: 31 men and 30 women (median age, 67.5 years). Eighteen subjects had type 1 diabetes and 43 had type 2 diabetes, with a median disease length at baseline of 19 years (range, 14 to 28 years). Median follow-up was 70 months, ranging from 57 to 72 months.
The rate of MACCE
The prevalence of any findings at whole-body MRI was considered high (66%) by the authors. In addition, the prevalence of findings was similar between cardiovascular (36%), cerebrovascular (39%), and peripheral vessel imaging (43%).
Breaking down the results further, positive late gadolinium enhancement in any myocardial segment had the highest prevalence (28%) among cardiac findings, while an abnormal amount of white-matter lesions had the highest prevalence among cerebrovascular findings (23%).
The median time between whole-body MRI and the first major adverse cardiac and cerebrovascular event was 35 months, ranging from 10 to 58 months. The absence of any pathologic finding in diabetic patients was associated with a zero probably of a future event during follow-up. Furthermore, the presence of any detectable ischemic and/or atherosclerotic changes at whole-body MRI was associated with a MACCE rate of 20% at three years and 35% at six years.
As one might expect, patients who experienced a MACCE were more inclined to have abnormal cardiac, carotid, and peripheral vessel MRI results than those who had no adverse events.
During follow-up, 14 patients experienced a MACCE, and among this group, there were six deaths (43%): five from a heart attack and one from a stroke. In addition, four patients died from noncardiac-cerebrovascular causes.
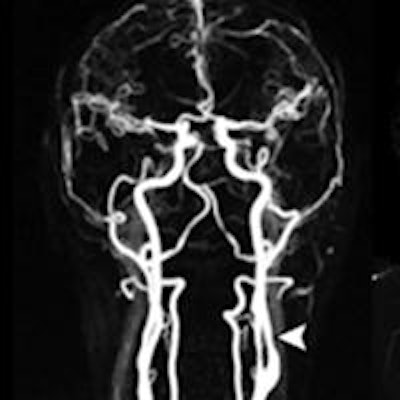
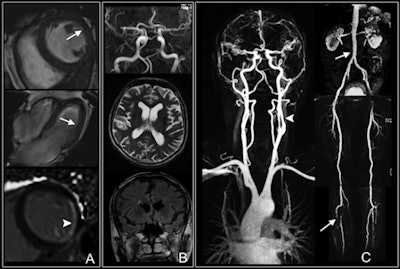 Whole-body MRI shows multiple findings in a 74-year-old man with type 2 diabetes for 21 years. Cardiac images (A) show impaired function with anterolateral hypokinesia (arrows). Late gadolinium-enhanced image (bottom) shows enhancement of anterolateral myocardium (arrowhead) indicative of myocardial infarction. Cerebral images (B) show normal cerebral arteries. Vascular images (C) demonstrate 50% stenosis of left internal carotid artery (arrowhead) and luminal irregularities of the abdomen (upper arrow), thighs, and lower leg with severe atherosclerotic disease and vessel occlusion (lower arrow). Images courtesy of Radiology.
Whole-body MRI shows multiple findings in a 74-year-old man with type 2 diabetes for 21 years. Cardiac images (A) show impaired function with anterolateral hypokinesia (arrows). Late gadolinium-enhanced image (bottom) shows enhancement of anterolateral myocardium (arrowhead) indicative of myocardial infarction. Cerebral images (B) show normal cerebral arteries. Vascular images (C) demonstrate 50% stenosis of left internal carotid artery (arrowhead) and luminal irregularities of the abdomen (upper arrow), thighs, and lower leg with severe atherosclerotic disease and vessel occlusion (lower arrow). Images courtesy of Radiology.The initial study results suggest whole-body MRI can provide "strong prognostic information" about diabetic patients and their potential for a heart attack or stroke, the authors concluded.
Because the results are "encouraging but very early," Bamberg's facility provides these types of whole-body MRI exams for research purposes only. "I anticipate that the clinical demand for such whole-body MR scans will certainly increase, once our findings have been replicated in larger trials," he said.
Bamberg and colleagues plan to continue their research and validate the results and findings to date.
"Certainly, the results are ... encouraging and the potential clinical impact is tremendous," he added. "I also feel that patients with diabetes are highly keen and motivated in optimizing their treatment and prognosis. A tool that assesses the degree of systemic subclinical disease in a disease that is affecting the whole-body is just a unique opportunity."



















