3D whole-heart myocardial perfusion cardiac MRI (CMR) at 3 tesla accurately detects functionally significant coronary artery disease with results that are comparable to more invasive techniques, according to study published online on 18 July in the Journal of the American College of Cardiology.
Cardiac MRI has advantages over SPECT, the conventional method for assessing myocardial perfusion, such as higher resolution and a lack of ionizing radiation, the authors noted. But a drawback to traditionally used 2D CMR methods has been that they cover the heart with a limited number of contiguous slices, which limits diagnostic yield and affects the quantification of ischemic burden.
New second-generation 3D cardiac MRI techniques could overcome this deficiency, and are particularly promising when conducted at more powerful 3-tesla field strengths, according to a team led by Dr. Roy Jogiya from King's College London and colleagues from several centers in London, Zurich, and Leeds, U.K.
Comparisons to the gold standard
The authors sought to test the viability of 3D CMR at 3 tesla by comparing it to fractional flow reserve (FFR), which assesses the severity of coronary stenosis by using angiography to insert a wire in the heart to acquire pressure measurements. FFR levels less than 0.75 correlate closely with objective evidence of reversible ischemia, the authors wrote.
In a secondary aim, the authors wanted to determine cardiac MRI's ability to assess the extent of myocardium that is at risk. For this task, they compared CMR measurements to the Duke jeopardy score (DJS), which is derived by dividing the coronary tree into six segments, and all segments distal to 70% or more stenosis based on angiography exams are considered to be at risk.
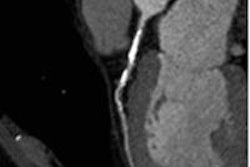
The JACC study examined 53 patients referred for angiography who underwent rest and adenosine stress 3D whole-heart myocardial perfusion 3-tesla CMR. All patients were scanned on a 3-tesla MRI system (Achieva, Philips Healthcare); stress perfusion images were acquired during adenosine-induced hyperemia.
FFR was calculated and performed in all coronary arteries with luminal stenosis of 50% or more in two orthogonal views, with FFR of less than 0.75 deemed to represent hemodymically significant stenosis. Coronary angiograms were used to calculate DJS to quantify the myocardium at risk, the authors wrote.
A reader blinded to the results examined angiographic images using quantitative catheter angiography; significant coronary artery disease was defined as 70% stenosis of the left anterior descending (LAD), circumflex, or right coronary arteries (RCA) with a luminal diameter of 2 mm or smaller or stenosis of 50% or more in the left main stem.
Perfusion was scored visually both per patient and by coronary territory, and ischemic burden was calculated by quantitative segmentation of the volume of hypoenhancement.
FFR was measured in 64 of 159 coronary vessels, 39 of which had an FFR of less than 0.75. The overall disease prevalence in the study population was 64% with 72 (45%) of the vessels analyzed containing 50% or more diameter stenosis.
3D CMR vs. FFR for detecting coronary artery disease
|
The study showed excellent agreement between FFR and 3D whole-heart myocardial perfusion CMR, and higher specificity than a previous study comparing 3D CMR with quantitative coronary angiography, though sensitivity was the same at 91%, the study team wrote.
Receiver operating characteristic (ROC) analysis showed an area under the curve of 0.89 (95% confidence interval [CI]: 0.785 to 0.991; p < 0.001). Quantitative coronary angiography performed in all vessels showed none with 50% or more stenosis that was not detected by FFR, Jogiya and colleagues wrote. In vessels with an FFR of 0.75 or more, mean diameter stenosis was 48.7%; in vessels with an FFR of less than 0.75, the mean diameter stenosis was 75.6%.
In the comparison with the Duke jeopardy score, Pearson's correlation coefficient showed a strong correlation (r = 0.82; 95% CI: 0.70 to 0.89) between the DJS and ischemic volume on cardiac MR (p < 0.0001), Joiya and colleagues reported. When the analysis was limited to patients correctly identified by CMR (48 of 53), the correlation rose to r = 0.87 (95% CI: 0.78 to 0.93; p < 0.0001).
Whole-heart myocardial perfusion CMR accurately predicts the presence of hemodynamically significant coronary artery stenosis as measured using FFR, and shows close agreement between estimates of ischemic volume with an invasive index of ischemic burden as represented by the Duke jeopardy score, Jogiya and colleagues concluded.
"3D acquisition methods overcome some of the remaining limitations of myocardial perfusion CMR; specifically, the limited myocardial coverage offered by conventionally used 2D," they wrote. "Furthermore, 3D acquisition is more signal-to-noise efficient than 2D imaging; in addition, because all data are acquired in one shot, all images are acquired in the same cardiac phase."
A principal limitation of the study was the high disease prevalence of the study population, the group noted. In addition, FFR was measured only in vessels with 50% or more stenosis.
"Multicenter studies to determine the use of 3D myocardial perfusion CMR as a noninvasive strategy for the diagnosis and risk stratification of patients with suspected CAD seem warranted," they wrote.
In an editorial accompanying the study, Dr. Jens Vogel-Claussen from the Hannover Medical School in Hannover, Germany, wrote that the extensive advances that have come with 3D CMR at higher-strength 3-tesla imaging will likely make myocardial stress perfusion CMR even more competitive with other stress perfusion imaging tests like SPECT and PET.
For the 3D technique to become dominant, however, "future trials have to show that this novel 3D MRI perfusion technique at 3 tesla is robust and can be applied in a multicenter setting including various MRI vendors," Vogel-Claussen wrote. "Also, the feasibility and potential clinical application of quantitative 3D MRI perfusion measurements in ischemic and nonischemic heart disease -- as already shown with 2D perfusion MRI and PET -- has to be evaluated in future research."