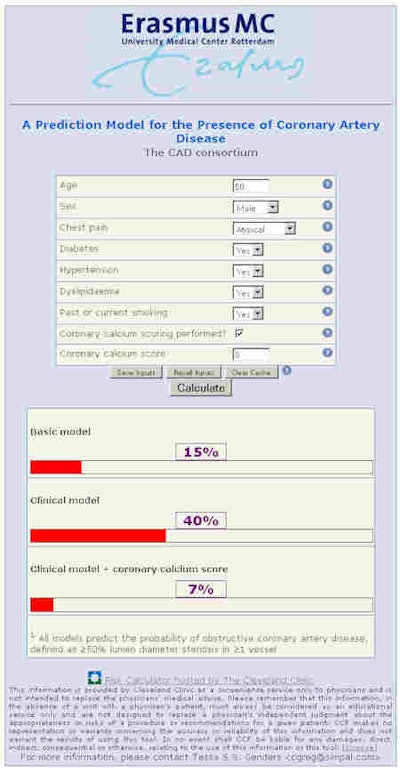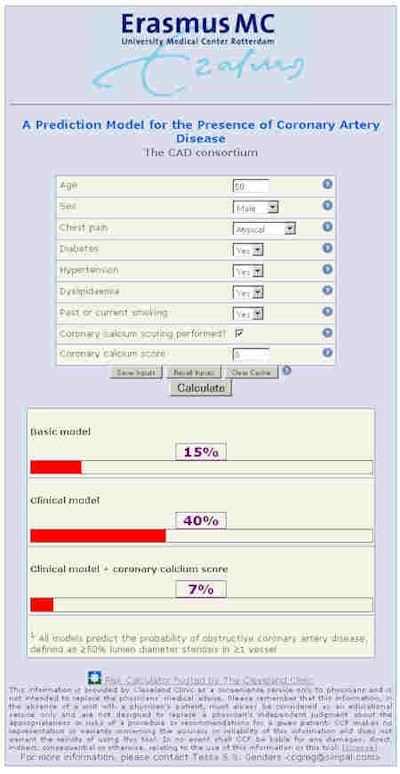
A new Web-based prediction tool can help identify patients at high risk of coronary artery disease. The model, developed by 18 hospitals in Europe and the U.S., outperforms the most widely used risk models for predicting coronary artery disease in low-risk patients with new-onset chest pain, according to a leading Dutch socioeconomic expert.
Although the new model's performance is improved significantly with coronary artery calcium (CAC) score results, it still permits effective disease risk assessment without CAC, ECG, or other clinical exam results, thus simplifying the task of risk assessment for primary care providers. Reportedly, the online calculator can be easily integrated into electronic patient record or mobile applications.
The research consortium found that age, sex, symptoms, and coronary calcium score were strong predictors of coronary artery disease, predicting probabilities that ranged from 2% for a 50-year-old woman with nonspecific chest pain and no risk factors, to 91% for an 80-year-old-man with typical chest pain and multiple risk factors. Better risk prediction models are needed since only 41% of patients undergoing catheter-based coronary angiography are found to have obstructive coronary artery disease, Dr. Myriam Hunink, PhD, a professor of radiology and epidemiology at Rotterdam's Erasmus Medical Center, and colleagues wrote in the British Medical Journal published online on 12 June 2012.
The best noninvasive assessment method to date, the Duke clinical risk score, is known to overestimate the probability of coronary artery disease, they noted. The new Erasmus model, developed and validated based on data from more than 5,000 patients, includes hypertension as a predictor and does not rely on echocardiography findings, stated Hunink et al. It permits doctors to make better decisions in selecting the best diagnostic test in a particular patient, and decide on further management based on the results.
"We perceived a need for an updated and stepwise approach to estimate the probability of coronary artery disease in patients with new onset of chest pain in a low prevalence population as clinical information and test results become available, in particular because implementation of the guidelines needs calculation of the pretest probability," Hunink noted. "Therefore, we aimed to estimate the probability of obstructive coronary artery disease on the basis of clinical presentation and cardiovascular risk factors, and to determine the incremental diagnostic value of exercise electrocardiography and the coronary calcium score."
The study team formed a consortium in which each hospital with a database of at least 80 eligible patients enrolled in single-center studies. Part of the European network for the assessment of imaging in medicine, the consortium aimed to perform pooled analyses of existing prospective data in order to improve their statistical power and increase the generalizability of their results.
"Primary outcome was obstructive coronary artery disease, defined as at least one vessel with at least 50% diameter stenosis found on catheter based coronary angiography," they wrote. "Since we combined existing databases from different hospitals, CT-based and catheter-based coronary angiographies were performed at each institution according to local protocols; we allowed both visual assessment and quantitative assessment for the interpretation of results for these procedures."
To participate, institutions had to have an existing database of at least 80 low-risk chest pain patients. Eligible patients presented with stable chest pain and were referred for conventional catheter-based or CT angiography. Patients with a history of myocardial infarction or previous revascularization were excluded.
Fourteen of the datasets consisted of consecutive patients enrolled in prospective studies for other research objectives. Four consisted of patients identified retrospectively as eligible via electronic radiology reporting systems. The study team evaluated inclusion and exclusion criteria and obtained missing information from records.
The group collected data on age, gender, symptoms, risk factors for cardiovascular disease, tests results, and the presence of coronary artery disease. They defined "typical" chest pain as substernal chest pain or discomfort that is provoked by exertion or emotional stress, and relieved by rest or nitroglycerine, or both. Atypical chest pain was defined as having two of the above three criteria, and if none of the criteria was present, symptoms were categorized as nonspecific.
"In our study, only a minority of patients underwent catheter-based coronary angiography," Hunink et al stated. "An analysis restricted to patients who underwent catheter-based coronary angiography could have been influenced by verification bias. Therefore, we imputed data for catheter-based coronary angiography by using the CT-based procedure as an auxiliary variable, in addition to all other predictors."
Results for the two procedures correlate well, especially in patients who are negative at coronary CTA, and this was confirmed in 1,609 patients who underwent both procedures (Pearson r = 0.72), the group reported. Since coronary CT angiography (CCTA) data were used for imputation, its results were not included as a predictor in the model.
The performance of the Duke clinical score was evaluated based on published data predicting 75% stenosis. Resting echocardiogram was assumed to be normal since patients had no history of coronary disease. The authors plotted the predicted probability with the observed proportions of severe disease (≥70% stenosis or ≥50% left main stenosis).
The study defined three prediction models:
- A basic model including age, sex, symptoms, and setting
- A clinical model including age, sex, symptoms, setting, diabetes, hypertension, dyslipidemia, smoking, and body mass index
- An extended model including all clinical variables and the coronary calcium score
The risk model was populated with all known significant clinical predictors of coronary artery disease in a multivariable, random effects, logistic regression model, while nonsignificant predictors (odds ratio < 1.01) of disease were omitted, the authors wrote. Availability of exercise echocardiography data was limited.
"We intended to apply our prediction models to patients in low prevalence populations, for whom the best diagnostic management should be determined based on an estimated pretest probability," Hunink et al wrote. "By contrast, all patients in the high prevalence setting had a clinical indication for catheter-based coronary angiography, in whom estimating the pretest probability would not be relevant to them. However, because it would be inefficient to derive a prediction model in a low prevalence population only (since most patients will not undergo the reference standard), we also included databases with patients referred for catheter-based coronary angiography. These data provided valuable information on the correlations between clinical presentation, risk factors, and the two angiography procedures, which was essential for reliable imputation of covariables and outcomes in the low prevalence populations."
Differences between low- and high-yield prevalence settings were tested, along with interactions between symptoms and sex, symptoms and age, and symptoms and diabetes, they wrote. The validity of the clinical model was also evaluated in a cross-validation procedure.
The study population included 5,677 patients (3,283 men mean age 58 years, and 2,394 women mean age 60 years). Ninety-one percent (n = 5,190) underwent catheter-based CTA, revealing obstructive disease in 31% of patients (n = 1,634). Of these patients, 66% (n = 1,083) underwent catheter-based coronary angiography, which showed positive results in 82% (n = 886).
In 3,556 patients without obstructive disease on CT based coronary angiography, 526 (15%) underwent catheter-based coronary angiography, which showed negative results in 498 (95%). Overall, 2,062 (36%) patients underwent catheter-based coronary angiography, with 1,176 (57%) diagnosed with obstructive coronary artery disease. Missing values occurred in four (0.1%) patients for age, six (0.1%) for symptoms, 126 (2.2%) for hypertension, 189 (3.3%) for diabetes, 187 (3.3%) for dyslipidemia, 155 (2.7%) for smoking, 354 (6.2%) for body mass index, and 810 (14%) for coronary calcium score.
Of the 3,556 patients without obstructive disease at coronary CTA, 15% underwent catheter-based angiography, which was negative in 97-98.4% of cases across multiple imputations. There were 1,634 with obstructive disease at CCTA, of which 34% did not undergo invasive coronary angiography. Those who did were positive in 65-77% of cases.
Results in the clinical model showed that all predictors except BMI were significantly associated with obstructive coronary artery disease.
"The clinical model improved the prediction, compared with the basic model," they wrote. "Whereas an abnormal exercise electrocardiography had limited predictive value in the multivariable prediction model, the coronary calcium score was a major predictor, which increased the c statistic from 0.79 to 0.88. Most predictor effects decreased after addition of the coronary calcium score; dyslipidemia and smoking were no longer significant. We obtained similar results when using CT-based coronary angiography as the outcome in patients who did not undergo catheter-based coronary angiography."
Abnormal exercise electrocardiography had limited predictive value in the multivariable prediction model, however, the coronary calcium score was a major predictor. Most predictor effects decreased after addition of the coronary calcium score, and dyslipidemia and smoking were no longer significant, the authors wrote. CT-based coronary angiography produced outcomes similar to those of catheter-based coronary angiography.
Logistic recalibration showed no significant differences between the overall hospital-specific effects of the disease predictors compared with the overall effects of these predictors in the clinical model, the group reported.
"With recently collected data and modern statistical methods, we developed a prediction model that performed well in estimating the probability of coronary artery disease," Hunink et al wrote. "The need for an updated model was evident by our results showing that the Duke clinical score significantly overestimated the probability of coronary artery disease. Age, sex, symptoms, and coronary calcium score were strong predictors for disease. The clinical model predicted probabilities between 2% for a 50-year-old woman with nonspecific chest pain without any risk factors, and 91% for an 80-year-old man with typical chest pain and multiple risk factors."
Despite its limitations, current guidelines still recommend the use of Diamond and Forrester's 1979 prediction model, which showed the importance of age, sex, and symptoms, they wrote. The Duke clinical model developed in 1993, predicted the presence of at least 75% stenosis based on age, sex, symptoms, history of myocardial infarction, smoking, dyslipidemia, diabetes, and resting electrocardiography. This study showed that the Duke score overestimated the probability of coronary artery disease, the authors wrote.
Among its limitations, the study relied on databases from other studies that relied on varying research objectives, according to the authors, who also noted that patient selection and evaluation on the basis of test results could lead to verification or selective-referral bias.
"We believe that our model improves the estimate of the pretest probability" compared with the Duke Clinical score, and unlike the Duke score, it was developed from data at several hospitals, the group wrote. "Our model does not need inclusion of resting electrocardiography findings, which could be convenient in primary practice."
"A refined estimate of the probability of coronary artery disease allows doctors to make better decisions as to which diagnostic test is best in a particular patient ... and to decide on further management based on the results of such tests," Hunink et al wrote. "Our stepwise models can be used to evaluate the added value of performing coronary calcium score either before performing the test or after obtaining the calcium score."
The analysis shows that the coronary artery calcium score significantly improves the estimate of the probability of coronary artery disease, suggesting that it should be considered for patients with chest pain." The results also confirm the limited utility of exercise echocardiography, though many physicians still consider it important for clinical practice.
"Prediction tools are useful only when they are easily accessible at the point of care, which is why we designed an online calculator," the authors wrote. "The calculator could be implemented in electronic patient records, electronic order entry systems, or smartphone or tablet applications."
The online calculator is below and can be accessed by clicking here.