In a cardiovascular study with relevance to today's emerging lung cancer screening programs, Finnish researchers report that calcium detected incidentally at chest CT predicts death from cardiovascular disease and from all causes.
And they warn that doctors who ignore such findings may be putting their patients at risk of early death.
In more than 500 individuals scanned with chest CT and followed for 10 years, the researchers found that calcifications in the aortic arch and those of brachiocephalic origin are independent predictors of all-cause deaths, while left anterior descending artery and brachiocephalic calcifications were independent predictors of cardiovascular deaths, as reported in Acta Radiologica (3 July 2012).
Many patients die of sudden cardiac death without the benefit of specialized CT scans, such as coronary CT angiography, or coronary artery calcium (CAC) tests, which are known to reliably predict cardiac disease risk, the study authors wrote.
But that doesn't mean these patients never see the inside of a CT scanner. According to study author Dr. Tapio Vehmas and colleagues from the Finnish Institute of Occupational Health in Helsinki, many patients at risk undergo routine chest CT scans from which calcifications can be detected and used to assess coronary artery disease risk. For example, in the U.S. more than 10 million individuals undergo chest CT scans each year, they said.
"Patients subjected to chest or body CTs are exposed to a considerable radiation burden," Vehmas and colleagues wrote. "Their imaging data should be comprehensively evaluated to maximize the benefit from these expensive examinations and to justify the radiation load."
Knowledge of arterial calcifications from chest CT could be used to estimate a patient's risk of cardiovascular disease and guide further exams, preventive measures, and early treatment, and evaluation of calcifications "must be based on visual estimations in these nonspecial CT studies," they wrote.
The authors explored the death risk associated with visually scored arterial calcifications found as secondary findings in nongated ordinary chest CTs.
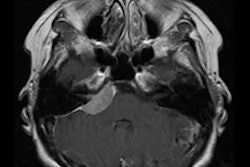
The retrospective study examined a total of 504 men (ages 39-81 years, mean 63 years) who were previously screened for lung cancer with spiral CT and later visually scored for atherosclerotic calcifications in the aorta, the origin of its great branches, and the coronary arteries. The Finnish National Register of Causes of Death was used to check the mortality of these individuals at a mean 10.4 years (range 0.25-13.0 years) of follow-up.
All patients underwent a single-detector unenhanced chest spiral CT (Picker PQ 2000, Philips Healthcare) in the supine position with breath-hold (10-mm-slice reconstructions, 125 mA, 140 kV, 10-mm collimation, pitch 1.5). Images were read for calcium at the right coronary artery, left anterior descending artery, left circumflex artery, and aorta (ascending, arch, and descending) and in the precervical arteries (origins of the brachiocephalic trunk, left carotid, and left subclavian arteries), the group reported.
A total of 160 deaths (31.7%) occurred among the 504 patients, including 57 due to cardiovascular disease (33 from ischemic heart disease, 16 from cerebrovascular disease, eight from other cardiovascular causes). Thus, cardiovascular deaths formed 35.6% of all deaths encountered in this population.
The average calcium scores at all anatomic sites were significantly higher among those who died, but these individuals were also older and had longer smoking histories than those who survived, the authors noted.
Calcifications at several anatomic sites significantly predicted both all-cause and cardiovascular deaths in the enter models. Calcifications in the aortic arch (hazard ratio [HR] = 1.35, 95% confidence interval [CI]: 1.08-1.69, p = 0.009) and the brachiocephalic origin (HR = 1.45, CI: 1.15-1.82 p = 0.002) remained independent predictors of all-cause deaths.
Regarding cardiovascular deaths, calcifications in the left anterior descending artery (HR = 1.86, CI: 1.29-2.67, p = 0.001) and brachiocephalic calcifications (HR = 1.65, CI: 1.09-2.49, p = 0.018) also were independent predictors.
"Cardiovascular deaths were significantly predicted by calcifications in the left-side coronary arteries and by the coronary sum score; by calcifications in the aortic arch [and] the descending aorta and [by the] aortic sum score; by calcifications in the base of the brachiocephalic artery; and by the grand sum of all calcifications," Vehmas and colleagues wrote.
In the backward model, left anterior descending artery and brachiocephalic calcifications were significant calcification predictors of cardiovascular deaths, they added.
"The study found a clear relation, independent of covariates, between visually scored chest atherosclerotic calcifications at several sites and both all-cause and cardiovascular deaths," the researchers concluded. "All results were in line with each other, and the multiple comparisons performed were therefore hardly a problem."
The same relationships were less clear for cerebrovascular disease, likely due to the limited number of deaths and the lack of statistical power, the group added.
Few papers deal with incidentally detected calcifications, the researchers noted. But Shemesh et al, for example, found that the rate of cardiovascular deaths increased with rising CAC scores (Radiology, November 2010, Vol. 257:2, pp. 541-548). Thoracic aorta calcifications have been associated with an increased risk of death and cardiovascular events, but the predictive value was limited. In this study, deaths were predicted at several anatomic sites.
"Arterial calcifications occurred in more than 90% of subjects and were related to age, blood pressure, erythrocyte sedimentation rate, and smoking," they wrote. Intra- and interclass correlation between observers ranking vessel calcifications were almost all good or excellent, and the follow-up time also was longer than found in most other studies.
Importantly, they said, these close relationships between calcification and death were demonstrated using outdated single-slice CT technology; modern scanners are expected to show even stronger associations.
Physicians should pay attention to chest atherosclerotic calcifications and actively report the findings even if they're not related to the original indication for the scan, the authors wrote.
With careful reporting, patients at cardiovascular risk may thus be identified at an early stage of their atherosclerotic disease, according to the authors. "This policy could maximize the benefit gained from chest CT examinations," they wrote, and, in particular, the value of CT lung screening.
More study is needed to assess the value of interventions after finding incidental arterial calcifications, they added.