French researchers have found that MR volumetric measurements are reliable indicators of rectal cancer prognosis and can help predict disease-free survival and tumor regression, according to a study published online on 21 March in Radiology.
The information obtained from MR volumetric measurements could help guide patient treatment, especially in low-lying tumors, which are more difficult to assess, and help predict therapy outcome, noted lead author Dr. Stephanie Nougaret, from the department of abdominal imaging at Saint Eloi University Hospital in Montpellier, France.
The researchers explored the facility's database from May 2004 to May 2008 for patients with pathologically proven rectal adenocarcinoma. The search found 58 consecutive patients -- 44 men and 14 women -- with a mean age of 58 years (ranging from 37 to 78 years) to participate in the study. The subjects had histologically confirmed low- or midrectal adenocarcinoma and, among other inclusion criteria, had undergone an MRI prior to and after chemotherapy and radiation treatment and surgical resection.
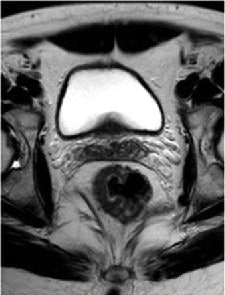
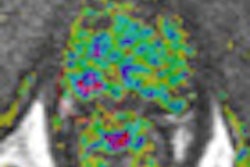
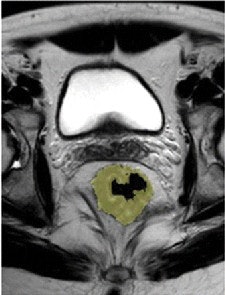 T2-weighted fast spin-echo axial oblique MR image (left) and tumor volumetric image (right) of a 54-year-old man before chemotherapy/radiation treatment. Pretreatment volume was 54 cm3. All images courtesy of Radiology.
T2-weighted fast spin-echo axial oblique MR image (left) and tumor volumetric image (right) of a 54-year-old man before chemotherapy/radiation treatment. Pretreatment volume was 54 cm3. All images courtesy of Radiology.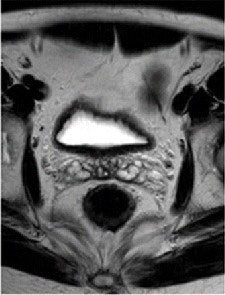
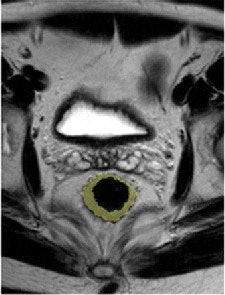 After therapy, the T2-weighted fast spin-echo axial oblique MR image (left) and tumor volumetric image (right) show no tumor response in the same patient. Post-treatment tumor volume was 45 cm3.
After therapy, the T2-weighted fast spin-echo axial oblique MR image (left) and tumor volumetric image (right) show no tumor response in the same patient. Post-treatment tumor volume was 45 cm3.Prior to treatment, 42 of the 58 patients (72%) had a low-rectal tumor, with the distal extent of the tumor 5 cm above the anorectal ring. The remaining 16 patients (28%) had midrectal tumors, which were 5 to 10 cm above the anorectal ring.
All 58 patients received 3D conformal treatment planning and preoperative radiation therapy at a dose of 45 Gy, which was delivered to the pelvis and 25 fractions in 28 patients. There were 23 patients who received a dose of 5.4 Gy in three fractions and in a limited volume. Seven patients received a high dose of radiation therapy of 63 Gy.
Pre- and post-treatment MRI was performed with a 1.5-tesla system (Intera R10, Philips Healthcare) using an eight-element pelvic phased-array surface coil. The subjects were imaged in the prone position after the placement of a thin rectal catheter in the rectum.
After initial localization imaging, researchers acquired MR images of the pelvis and rectum, with T2-weighted images obtained in the transverse, coronal, and sagittal planes during the scanning time of approximately 30 minutes.
Two radiologists, who were blinded to clinical information about each patient, independently evaluated the images obtained before and after chemotherapy and radiation treatment.
Patient follow-up
The 58 patients received routine follow-up every three months for the first year, every six months for the next two years, and then yearly in the third year and beyond. During the follow-up visits, their conditions were evaluated through digital rectal exam, proctoscopy, chest x-ray, and serum carcinoembryonic antigen tests.
The mean follow-up of survivors at the time of analysis was 52 months. Two patients were lost to follow-up and five individuals had metastatic disease at the time of diagnosis.
The MR images calculated the mean tumor volume was 58 cm3 ± 75 before chemotherapy/radiation treatment and 20 cm3 ± 31 after therapy. The mean tumor volume reduction ratio in all patients was 68% ± 23.
Downstaging occurred in 33 of the 58 patients (57%). The tumor volume reduction rates after chemotherapy/radiation treatment were significantly different between patients whose tumors were downstaged and those whose tumors were not downstaged (P < .0001). There also was no significant difference based on tumor location.
Disease-free survival
In evaluating disease-free survival rates, the researchers found that 16 of the 51 patients (31%) had recurrence after a mean of 20 months ± 10 months. Among those 16 subjects, 13 people had low-lying tumor.
The most common type of first recurrence was hepatic metastases, which was discovered in nine patients (56% of patients with recurrence). Other sites of relapse included local recurrence within the pelvis among four individuals, lung metastases in two participants, and peritoneal disease in one case.
There were 12 recurrences, which were asymptomatic and detected by MRI during routine follow-up, with two additional cases of increasing carcinoembryonic antigen levels.
Tumor regression grade
In addition, 34 of the 58 patients (59%) had a tumor regression grade (TRG) of 1 or 2, while 24 individuals (41%) had a tumor regression grade of 3 or 4.
Researchers also found tumor volume reduction rates after chemotherapy/radiation treatment were significantly different between patients with TRG 1 or 2 and subjects with TRG 3 or 4. "The mean tumor volume reduction was 57 cm3 ± 20 in patients with TRG 1 or 2 and 83 cm3 ± 18 in individuals with TRG 3 or 4 (P < .0001)," they wrote, adding there were no significant differences seen according to the location of the tumor.
Nougaret and colleagues also found that 25 of the 58 patients (43%) had a total volume reduction rate of at least 70%, while 33 individuals (57%) had a total volume reduction rate of less than 70%.
"A tumor volume reduction of at least 70% was significantly associated with good histologic regression (TRG 3 or 4) (P < .0001)," they added, "with an accuracy of 74% (43 of 58 patients), a positive predictive value of 88% (22 of 25 patients), and a negative predictive value of 64% (21 of 33 patients)."
Based on the results, Nougaret and colleagues concluded that "volumetric measurements are reliable markers of rectal cancer prognosis, enabling the prediction of [disease-free survival] and TRG. The cutoff of 70% is an easy parameter to use as a surrogate for clinical response to predict both TRG and outcome."