VIENNA - Being diagnosed with rectal cancer not only means the likely loss of a rectum, but also the odds are unpleasantly high that it will be a death sentence. Advanced imaging techniques, however, are offering new options to low-risk patients and more hope for survival to high-risk ones. Radiologists collaborating with radiation oncologists have the potential to make a world of difference for these patients.
Dr. Vincenzo Valentini, president of the European Society for Radiotherapy and Oncology (ESTRO) and a radiation oncologist at the Università Cattolica S. Cuore in Rome, is an enthusiastic supporter of multispecialty cancer treatment teams. In this new era of individualized treatment for rectal cancer patients, he believes that adoption of theranostic imaging is essential.
Theranostic imaging, as defined by Prof. Søren M. Bentzen, MD, of the University of Wisconsin Medical School's department of human oncology, in an article published in Lancet Oncology (2005, Vol. 6:2, pp. 112-117), refers to the use of information from medical images to determine how to treat individual patients. In the context of radiation oncology, theranostic imaging aims to map in three dimensions the distribution of a tumor, tissue, or functional feature, and to provide information about the clinical response of tumors or healthy tissues to radiotherapy.
 ESTRO President Dr. Vincenzo Valentini from Rome.
ESTRO President Dr. Vincenzo Valentini from Rome.
"In this visionary article, Prof. Bentzen predicted that theranostic imaging for radiation oncology will revolutionize the whole process of radiotherapy prescription and planning within five years. And he was correct," commented Valentini. "What he may not have wanted to predict was how intertwined the work of radiologists and radiation oncologists has become in this era of personalized treatment."
Valentini explained that when radiation oncologists established themselves as a distinct specialty from radiology many decades ago, relationships between the two professional groups were not always cordial. "At my hospital, radiologists and radiation oncologists began working closely together about 15 years ago. We increasingly became aware of how relevant imaging was to staging the treatment of cancer and its reaction to treatment, especially rectal cancer."
He said that radiation oncologists began to recognize that they could get better clinical results, and that radiologists realized that their contribution to treatment planning was vitally important. One of Valentini's goals as a co-chair of today's "ECR Meets" session is to emphasize to radiologists their importance not just with respect to the diagnosis of a patient, but also with respect to monitoring and contributing to the treatment plan for a rectal cancer patient.
Even when there is a willingness to work together, it is important that all team members of a therapeutic treatment team -- the oncologist, the surgeon, the radiation oncologist, and the medical physicist -- understand the terminology and the precise definitions of each other's specialty, he cautioned. Not only is communication important, it also must be accurately understood. The meaning of terminology, even when referring to the same anatomy, is not always the same. Valentini pointed out that ESTRO is starting to cosponsor multidisciplinary conferences and courses to bridge this gap.
Diagnostic imaging and the high-risk patient
From Dr. Gina Brown's perspective, over the past few years there's been a sea change in the management of rectal cancer. Diagnostic imaging has been of paramount importance to the abandonment of a one-size-fits-all approach.
Brown, a consultant radiologist at the Royal Marsden Hospital NHS Trust in Sutton, U.K., was the principal investigator of the MRI and Rectal Cancer European Equivalence Study (MERCURY), a multinational study that proved the importance of MRI examinations when staging a patient. The study showed that MRI images could predict outcome for patients who had completed initial chemoradiation therapy.
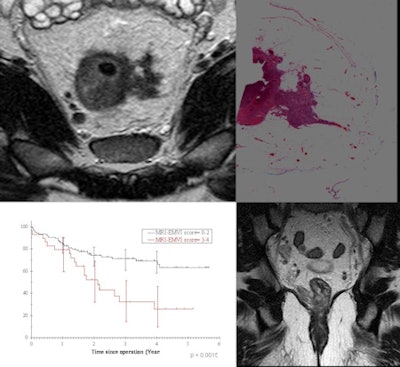 |
| MRI depicts the characteristic features of extramural venous invasion -- a poor prognostic factor seen in up to 30% of rectal cancer patients and associated with a 25% relapse-free survival. Detection of such high-risk patients may enable more intensive preoperative therapy and follow-up to reduce deaths related to metastatic disease. (Provided by Dr. Gina Brown) |
MRI exams have had an impact on how high-risk patients are staged by identifying features that place them at risk for metastatic disease. At the Royal Marsden, radiologists who identify biological risks shown on images that are known to cause local failure and or distant metastases to occur are part of a multidisciplinary team who evaluate if more aggressive treatment is needed.
"Careful staging of the tumor is vital. In 2003, we recognized that with a high-risk patient, it is worth the possibility of giving the type of systemic therapy that usually would follow surgery in advance of it. This type of systemic chemotherapy is very aggressive, with associated risks of unpleasant comorbidities and even mortality, but might eliminate metastases that exist at the time of diagnosis," Brown said.
 Dr. Gina Brown from Sutton.
Dr. Gina Brown from Sutton.
"From our outcome data, when tumors have spread more than 5 mm beyond the muscularis, there is a massive drop in disease-free survival and overall survival. A tumor invasion in the vein that can be identified by MRI is associated with only a 25% chance of disease-free survival. In addition to the aggressive therapy we prescribe from the findings in the original MRI exam, with regularly scheduled follow-up imaging, we can monitor the post-treatment outcomes. If disease occurs, such as liver metastasis, we can identify this promptly and remove it, giving the patient a better chance of longer survival," she added.
Brown hopes that her participation in today's panel will help equip radiologists with the knowledge to be able to spot high-risk tumors at the time that they are staged, thus positively influencing the treatment plan for the patient.
Adopting a 'wait-and-see' approach
Maastricht University Medical Center in the Netherlands is a pioneer in the adoption of an observation-only policy for patients with locally advanced rectal cancer who have a clinical complete response to neoadjuvant chemoradiotherapy. Advanced MRI and strictly adhered to patient follow-up is what makes colorectal surgeons and the therapeutic team confident about postponing total mesorectal excision (TME) until recurrence is detected.
In 2004, the demand of a patient who refused to have a TME performed when post-treatment MR images showed that his rectal cancer had completely disappeared launched the "wait-and-see" option at Maastricht. The patient, as well as his physicians, had read and been impressed with the outcomes of a landmark observational study of rectal cancer patients published that year conducted by Dr. Angelita Habr-Gamma at the University of São Paulo in Brazil.
Prof. Regina G.H. Beets-Tan, a Maastricht-based radiologist who subspecializes in oncologic and abdominal imaging, said that the surgeons and the patient's therapeutic management team were very open-minded about postponing surgery for qualified patients because they knew that modern MRI can help them in their clinical assessment of treatment response.
"Accurate assessment of response is very critical if organ-saving treatment like 'local excision' or 'wait and see' is being considered for patients with good response to neoadjuvant chemoradiotherapy. This information cannot be given with morphological MR imaging only. It is necessary to combine it with all the features of functional MRI imaging -- diffusion and perfusion MRI -- and get metabolic information from PET scans -- to be certain that there is no or small tumor burden left within the fibrosis," she noted.
In addition, the lymph nodes represent a risk. "You want to be sure that the patient has sterilized lymph nodes after chemoradiotherapy treatment, not to put the patient at risk for a nodal recurrence. We haven't solved this problem yet. Both endoluminal ultrasound (EUS), CT, and MRI lack sufficient accuracy for identifying nodal metastases, understaging by up to 25% for EUS and up to 16% for MRI. The problem is that in rectal cancer, the majority of metastatic nodes are smaller than 5 mm," she explained.
The radiology department at Maastricht investigates a lymph-node specific MRI contrast agent, gadofosveset trisodium, for nodal staging. A study of its use with rectal cancer patients showed it had a negative predictive value of more than 95% on a per-lesion basis and more than 85% on a per-patient basis, and suggested that patients with node-negative disease can possibly be identified.
At today's session, Beets-Tan plans to discuss how diagnostic imaging can better evaluate and monitor response of rectal cancer to preoperative chemoradiotherapy. Physicians tend to be reluctant to treat good responders without using surgery, mainly because of a lack of a sufficiently accurate technique to select them. The availability of such a tool will allow clinical trials that will prove whether organ-saving treatment is a safe alternative to surgery. If so, a paradigm shift in rectal cancer treatment will occur.
"Losing a rectum is devastating, and if this can be avoided with close monitoring of patients, it should be. Radiologists have the tools to support our clinicians, and we have the expertise."
Tailoring the radiotherapy approach
Prof. Karin Haustermans, chair of the department of radiation oncology of the cancer institute at Katholieke Universiteit Leuven in Belgium, is also a strong advocate of patient-tailored treatments. It is necessary to understand the molecular and biological mechanisms underlying tumor sensitivity and resistance to treatment, which can be done with the integration of molecular imaging, tumor, and blood markers.
 Prof. Karin Haustermans from Leuven.
Prof. Karin Haustermans from Leuven.
She recommends that consistent and reliable definitions of risk factors by detailed imaging assessment be implemented to facilitate this, and that standard protocols for advanced imaging procedures be established to ensure reproducibility of findings. In addition to using the TNM staging system, circumferential margin involvement, size of the primary tumor, and the location of the primary tumor in relation to the anal sphincter are important factors in making treatment decisions.
After determining what to irradiate and determining whether a short or long course of radiotherapy treatment is needed, it is important to determine if this standard is the optimal treatment for a patient. Haustermans stressed that patients with similar tumors might respond differently to a treatment. This could suggest a different tumor biology and microenvironment beyond the anatomical characteristics.
She noted that standard MRI can show findings that differentiate patients with a good prognosis from those at risk of distant metastases or those for whom there is a high risk of local recurrences and distant metastases.
"The use of PET/CT and diffusion-weighted MRI can increase the accuracy of metabolic responses to neoadjuvant chemotherapy treatments. But this information has been published in monocentric studies. I hope that multicenter trials will be set up to validate these findings. Before we can expect a widespread implementation of diffusion-weighted MRI and PET/CT into the daily clinical practice, we need multicenter trials that confirm these results in large patient populations. We need to demonstrate a benefit from this approach by objectively linking the ability to predict a response to a better treatment selection and, consequently, better outcome in all patients."
Originally published in ECR Today March 2, 2012.
Copyright © 2012 European Society of Radiology



















