As a first step toward the greater standardization of prostate imaging, the European Society of Urogenital Radiology (ESUR) has published a guideline for MRI of the prostate. The ESUR Prostate Working Group has developed a structured reporting system, called PI-RADS (prostate imaging, reporting, and data system), which has now been adopted by the American College of Radiology (ACR).
The role of MRI in prostate cancer evaluation continues to arouse controversy and is often underestimated. Technological advances over the past few years have demonstrated that multiparametric MRI, including diffusion-weighted imaging (DWI) and contrast-enhanced MRI, can better detect prostate cancer, evaluate the actual tumor burden, and is more accurate at tumor grading than standardized transrectal ultrasound biopsy protocols. Thus, multiparametric MRI can be used to evaluate tumor risk, leading to more tailored therapy.
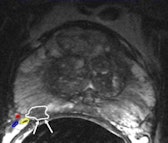
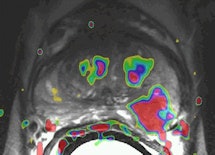 A 56-year-old male with prostate-specific antigen (PSA) level of 11; transrectal ultrasound (TRUS) biopsy, Gleason 3+4 left; DRE T1c. Prostatectomy confirmed Gleason 4+3 prostate cancer (PC) with extracapsular extension (ECE) in left peripheral zone (PZ). Left: Axial T2-weighted MR image shows low-signal lesion in the left PZ (white outline), which fits PC with ECE (arrow, PI-RADS 5). Right: Axial dynamic contrast-enhanced MR image shows asymmetric focal enhancement both in tumor in left PZ, with curve type 3 (PI-RADS 5). All images courtesy of Dr. Jelle Barentsz.
A 56-year-old male with prostate-specific antigen (PSA) level of 11; transrectal ultrasound (TRUS) biopsy, Gleason 3+4 left; DRE T1c. Prostatectomy confirmed Gleason 4+3 prostate cancer (PC) with extracapsular extension (ECE) in left peripheral zone (PZ). Left: Axial T2-weighted MR image shows low-signal lesion in the left PZ (white outline), which fits PC with ECE (arrow, PI-RADS 5). Right: Axial dynamic contrast-enhanced MR image shows asymmetric focal enhancement both in tumor in left PZ, with curve type 3 (PI-RADS 5). All images courtesy of Dr. Jelle Barentsz.Evidence is growing that MRI before the second, or even initial, biopsy can accurately distinguish between those patients who require immediate biopsies and those for whom biopsy can be deferred. A correlation between apparent diffusion coefficient (ADC), calculated from DWI, and Gleason score has been found. MRI before biopsy can help to detect high-grade tumors, which helps target biopsies within areas of low ADC values.
The ESUR's report was published online on 9 February by European Radiology. Lead author is Dr. Jelle Barentsz, a professor of diagnostic radiology at the University Hospital Nijmegen in the Netherlands and the chair of the Prostate MR-Center of Excellence.
The society's aim was to develop clinical guidelines for multiparametric MRI of the prostate by getting a group of prostate MRI experts to study the literature evidence and consensus expert opinion. True evidence-based guidelines could not be formulated, but a compromise, reflected by "minimal" and "optimal" requirements, was achieved, according to the authors. The scope of the guidelines is to promulgate high-quality MRI in acquisition and evaluation with the correct indications for prostate cancer across Europe, and eventually outside Europe. The guidelines for the optimal technique and protocols for detection, staging, and node and bone are presented. The use of endorectal coil versus pelvic phased-array coil and 1.5- versus 3-tesla are discussed. Clinical indications and a PI-RADS classification for structured reporting are presented.
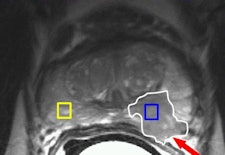
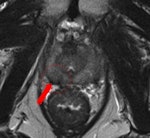
 A 48-year-old sexually active male with PSA 9; TRUS biopsy Gleason 4+3 PC at right PZ; stage T1c. Nerve-sparing prostatectomy was performed showing submillimeter ECE and negative resection margins. Postsurgery patient was potent and continent. Left: Axial T2-weighted MR image shows low signal tumor in right PZ (white area) with obliteration of the white fat at the rectoprostatic angle (arrows), indicating minimal ECE = PI-RADS 5. The NVB is indicated by red, blue, and yellow. Right: Nerve-sparing prostatectomy showed Gleason 4+3 PC with submillimeter ECE (T; blue area) at right PZ. Resection margins were negative. Patient was potent after surgery.
A 48-year-old sexually active male with PSA 9; TRUS biopsy Gleason 4+3 PC at right PZ; stage T1c. Nerve-sparing prostatectomy was performed showing submillimeter ECE and negative resection margins. Postsurgery patient was potent and continent. Left: Axial T2-weighted MR image shows low signal tumor in right PZ (white area) with obliteration of the white fat at the rectoprostatic angle (arrows), indicating minimal ECE = PI-RADS 5. The NVB is indicated by red, blue, and yellow. Right: Nerve-sparing prostatectomy showed Gleason 4+3 PC with submillimeter ECE (T; blue area) at right PZ. Resection margins were negative. Patient was potent after surgery.One in six men in their lifetime will be clinically diagnosed with prostate cancer, and this accounts for 350,000 cases, annually or 25% of all new male malignancies diagnosed in Europe, the authors noted. Currently, digital rectal examination, serum prostate specific antigen (PSA) -- a nonspecific blood test -- and transrectal ultrasound-guided biopsy -- where the target is mostly invisible -- are used as diagnostic tools.
"Advances in MRI show promise for improved detection and characterization of prostate cancer, using a multiparametric approach, which combines anatomical and functional data. Thus far, optimal acquisition and evaluation have not been agreed [upon], and as is often the case in clinical practice, it is not satisfactory to await conclusions from large-scale imaging and oncological trials," they stated.
The ESUR working group of prostate MRI experts had informal discussions at international congresses and by email. This crystallized into a series of specialist subgroups. The criteria for group inclusion were radiologists with at least three years of experience in prostate MRI (> 50 examinations per year), conducting research comparing image results with pathological specimens, coworking with urologists, and producing peer-reviewed international articles. Based on the recommendations of the subgroup chairs, a consensus document was established and finalized by two consensus meetings and email discussion.
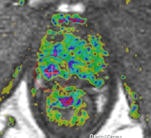
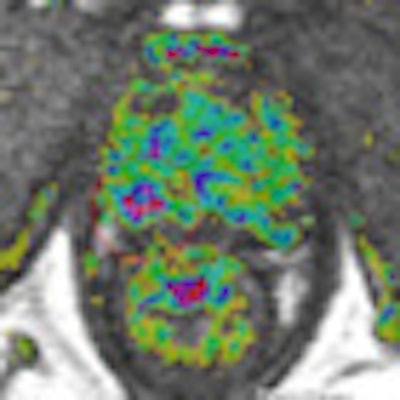
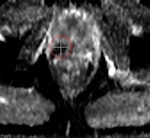 A 69-year-old male three years post electron-beam radiation therapy (EBRT, primary PC: Gleason 4+3 right PZ) with PSA increase to 2. MRI and TRUS-guided biopsy of this area confirmed Gleason 4+4 recurrence at right PZ (old tumor location). Left: Axial T2-weighted MR image shows low signal prostate due to previous EBRT. Therefore, tumor (arrow) is difficult to see. At arrow, there is some "bulging" (PI-RADS 5). Center: Axial DCE-MRI shows increased focal asymmetric contrast leakage at right PZ (circle, PI-RADS 5). Right: Axial ADC-map of DWI-MRI shows restriction (low signal, circle, PI-RADS 5). Final diagnosis: PI-RADS 5. TRUS biopsy of this area confirmed Gleason 4+4 recurrence.
A 69-year-old male three years post electron-beam radiation therapy (EBRT, primary PC: Gleason 4+3 right PZ) with PSA increase to 2. MRI and TRUS-guided biopsy of this area confirmed Gleason 4+4 recurrence at right PZ (old tumor location). Left: Axial T2-weighted MR image shows low signal prostate due to previous EBRT. Therefore, tumor (arrow) is difficult to see. At arrow, there is some "bulging" (PI-RADS 5). Center: Axial DCE-MRI shows increased focal asymmetric contrast leakage at right PZ (circle, PI-RADS 5). Right: Axial ADC-map of DWI-MRI shows restriction (low signal, circle, PI-RADS 5). Final diagnosis: PI-RADS 5. TRUS biopsy of this area confirmed Gleason 4+4 recurrence."Prostate imaging at 3-tesla benefits from higher signal-to-noise ratio and enables high-quality imaging within a short time without the use of an ERC [endorectal coil]. Data on 3-tesla for prostate cancer MRI are still conflicting. Thus, further research on this topic is needed," the authors noted. "Limitations of 3-tesla MRI are shorter T2- and longer T1-relaxation times, problems with susceptibility artifacts, dielectric effect, specific absorption rate, and the homogeneity of the magnetic field. However, hardware, multichannel coil, and parallel imaging technique improvements are currently solving most of these problems."
The ACR and ESUR are cooperating to design standards. The objective is to promote the transfer of MRI examinations from laboratories to patients, aiming to reduce unnecessary biopsies and treatment carried out on prostate cancer patients. MR PI-RADS will set the standards for prostate MRI reporting and help to combat prostate cancer by reducing unnecessary biopsies and focusing resources on those patients who truly need further treatment, according to Barentsz, who is the ESUR representative and co-chair of the MR PI-RADS ACR's Steering Committee.