Real-time elastography (RTE) is useful in assessing small testicular nodules and pseudonodules, which is relevant in clinical practice for managing testicular cancer, Italian researchers have found in a study published online first in European Radiology. Elastography is less relevant for larger lesions because most of them are malignant at clinical and ultrasound assessment.
Until B-mode ultrasound, physicians diagnosed scrotal lesions by palpation and changes in tissue consistency, which is problematic as assessment is related to the physician's experience and the lesion's size. As a solution, ultrasound has so far been considered the gold standard for evaluating scrotal abnormalities, but it doesn't provide a histological diagnosis.
Sonoelastography noninvasively measures mechanical properties of tissue, and images the elasticity of biological tissue. A portion of tissue is compressed and the degree to which it displaces is assessed. Real-time elastography was the first commercial ultrasound technique available for wide clinical applications, and its usefulness for diagnosing testicular lesions is being investigated.
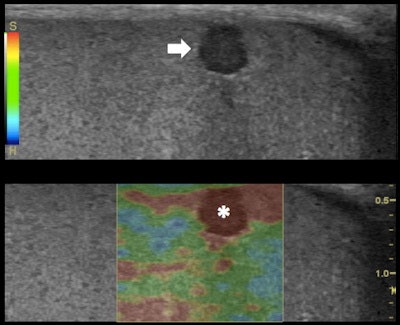 Top: Grayscale ultrasound longitudinal image of the testes: subcapsular 3-mm (in size) hypoechoic lesion (arrow). Bottom: RTE shows higher tissue displacement of the lesion (displayed in red) (*) compared with the testicular tissue (mainly displayed in green), suggesting a benign appearance: dense cyst. All images courtesy of Dr. Alfredo Goddi, SME-Diagnostica per Immagini Medical Center, Varese, Italy.
Top: Grayscale ultrasound longitudinal image of the testes: subcapsular 3-mm (in size) hypoechoic lesion (arrow). Bottom: RTE shows higher tissue displacement of the lesion (displayed in red) (*) compared with the testicular tissue (mainly displayed in green), suggesting a benign appearance: dense cyst. All images courtesy of Dr. Alfredo Goddi, SME-Diagnostica per Immagini Medical Center, Varese, Italy.
RTE evaluates the relative elasticity of different tissues by using a fast cross-correlation technique and a combined autocorrelation method. It creates an elastogram that is superimposed to the B-mode ultrasound image of the tissue and updated in real-time. The elastograms display a color-coded map of the relative elasticity -- stiffer areas are depicted as blue and softer areas are red; green indicates an intermediate level of elasticity.
Elastosonography is already used to assess breast, prostate, thyroid, and lymph node lesions, but few reports concerning the efficacy of RTE for scrotal mass assessment are available. In their preliminary study, Dr. Alfredo Goddi from SME-Diagnostica per Immagini Medical Center in Varese, Italy, and colleagues assessed RTE's ability to discriminate malignant from benign testicular lesions (Eur Radiol, 26 October 2011).
The study included 1,617 patients (mean age, 34; range, 2 months to 89 years) referred to the center's ultrasound department for scrotal abnormalities, with a total of 3,171 testicles examined by ultrasound. Lesions were found in 324 testicles, with ultrasound alone able to rule out tumors in 236 of them, eliminating the need for further exams. In the remaining 88 testicles, color Doppler ultrasound with RTE identified 144 lesions.
Three radiologists with more than 20 years of experience in scrotal ultrasound performed the exams. Elasticity images of the lesions were assigned the color-coded score of SCI to 5 suggested by Itoh et al (Radiology, May 2006, Vol. 239, pp. 341-350) according to the distribution of strain induced by light compression. Lesions were then assessed by shape, size, and score.
The researchers found 93.7% of all benign lesions showed a complete elastic pattern. Also, 92.9% of benign nodules smaller than 5 mm and 100% of the pseudonodules showed a nearly complete elastic pattern. Of the malignant nodules, 87.5% showed a stiff pattern. Sensitivity for RTE was 87.5%, specificity was 98.2%, and positive predictive value was 93.3%. Negative predictive value was 96.4%, and accuracy in differentiating malignant from benign lesions was 95.8%.
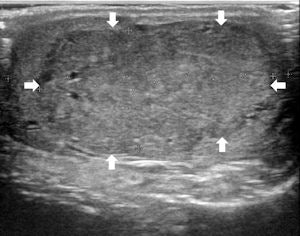
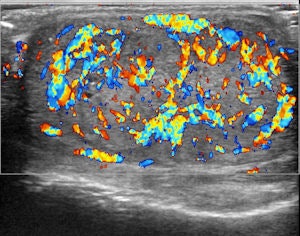
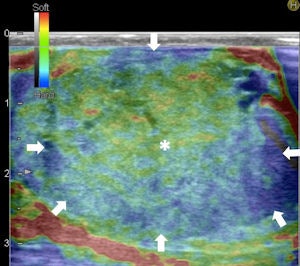
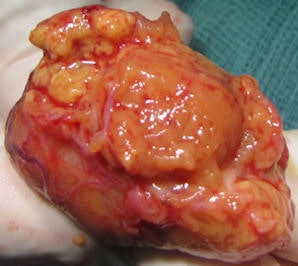 Top left: Grayscale ultrasound image of the testes showing a large isoechoic nodule (40 x 20 mm) compared with the testicular tissue (arrows). Top right: Color Doppler showing peripheral and central vascularization of the nodule, suggesting a malignant lesion. Bottom left: RTE of the nodule showing a large central strain area (mainly an intermediate elastic pattern displayed in green) (*) surrounded by a no-strain rim (the peripheral part of the lesion is blue) (arrows). This pattern, that the researchers suggested calling "score 3-inverted" (the opposite of the known color-coded score 3 reference of Itoh et al) seems to be related to the Leydig tumors. Bottom right: Gross specimen of the testicle. Histological diagnosis of the nodule was Leydig tumor, consisting of cells with abundant cytoplasm without interstitial fibrous stroma; the slow growth of the tumor induces sclerohyalinosis at the periphery. The tumor's macrostructure explains the RTE pattern.
Top left: Grayscale ultrasound image of the testes showing a large isoechoic nodule (40 x 20 mm) compared with the testicular tissue (arrows). Top right: Color Doppler showing peripheral and central vascularization of the nodule, suggesting a malignant lesion. Bottom left: RTE of the nodule showing a large central strain area (mainly an intermediate elastic pattern displayed in green) (*) surrounded by a no-strain rim (the peripheral part of the lesion is blue) (arrows). This pattern, that the researchers suggested calling "score 3-inverted" (the opposite of the known color-coded score 3 reference of Itoh et al) seems to be related to the Leydig tumors. Bottom right: Gross specimen of the testicle. Histological diagnosis of the nodule was Leydig tumor, consisting of cells with abundant cytoplasm without interstitial fibrous stroma; the slow growth of the tumor induces sclerohyalinosis at the periphery. The tumor's macrostructure explains the RTE pattern.Because clinical examination has its drawbacks, ultrasound has become the imaging technique of choice for evaluating scrotal abnormalities -- with the primary function of ultrasound being the diagnosis of a testicular mass to distinguish intratesticular from extratesticular location. Most extratesticular masses are benign, but intratesticular ones are malignant.
"Even though ultrasound is extremely sensitive, it does not offer any further information about the nature of the lesion, especially small ones," Goddi and colleagues wrote. "The detection of hypoechoic intratesticular lesions < 5 mm is not infrequent using transducers with a frequency range of 7.5-14 MHz or greater. It raises the issue of how to manage these nodules and how often and for how long these patients should be followed to exclude the tumoral nature of the nodules."
RTE evaluates relative tissue displacement after slight compression. The total amount of displacement used to compute the strain may be the sum of the external compression plus physiological patient motion -- even the minimal displacement of the testes due to the cremaster muscle contraction may contribute to the strain imaging, according to the authors.
In RTE evaluation, normal testicles mainly show a medium level of elasticity (displayed in green); some linear "red" structures within the testes are related to fluid component. Sometimes the glandular tissue below the tunica albuginea of the testicle presents less relative strain, displayed in light blue, probably due to the limited tissue displacement determined by the fibrous covering, the researchers wrote.
An elasticity score of 1 indicates lesions have the same compressibility of the surrounding tissue. RTE showed a prevalence of score 1 in 93.7% of the benign lesions and only one case with score 1 was found malignant.
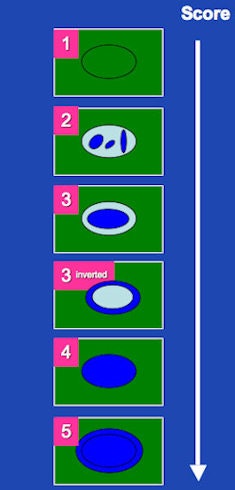 Color-coded elastographic score (SC1 to 5) suggested by Itoh et al for breast disease and modified by Goddi et al for testicular lesion assessment. 1 indicates strain for entire lesion. 2 indicates strain in most of the solid lesion with some areas of no strain. 3 indicates strain at the periphery of the solid lesion, with no strain at the center. 3-inverted indicates strain at the center of the solid lesion, with no strain at the periphery of the lesion. 4 indicates no strain in the entire lesion. 5 indicates no strain in the entire solid lesion and surrounding area. If scored between 1 and 3, lesion would be benign; if scored 3-inverted, lesion would be considered suspect for a Leydig tumor; if scored 4 or 5, lesion would be considered malignant.
Color-coded elastographic score (SC1 to 5) suggested by Itoh et al for breast disease and modified by Goddi et al for testicular lesion assessment. 1 indicates strain for entire lesion. 2 indicates strain in most of the solid lesion with some areas of no strain. 3 indicates strain at the periphery of the solid lesion, with no strain at the center. 3-inverted indicates strain at the center of the solid lesion, with no strain at the periphery of the lesion. 4 indicates no strain in the entire lesion. 5 indicates no strain in the entire solid lesion and surrounding area. If scored between 1 and 3, lesion would be benign; if scored 3-inverted, lesion would be considered suspect for a Leydig tumor; if scored 4 or 5, lesion would be considered malignant.
"Although our findings will require further confirmation, this result suggests that lesions with score 1, lesser than 10 mm, could be considered benign unless biochemical data/tumoral markers/hormonal levels suggest otherwise," the authors wrote.
Elasticity scores of 2 indicate lesions that are mainly soft, but have some stiff areas compared with the normal tissue. Assessing breast nodules, Itoh et al considered this pattern often characteristic of benign lesions such as fibroadenoma. In Itoh's study, only 21% of score 2 lesions were malignant. In the current study, 37.5% of score 2 lesions were malignant, two of which had a diameter larger than 11 mm.
"We suggest that when assessing scrotal lesions with such pattern (i.e., score 2), they should be considered suspicious until proven otherwise if larger than 11 mm and should be closely monitored if less than 10 mm diameter," Goddi's team wrote.
An elasticity score of 3 indicates strain at the periphery of a lesion with no strain at the center. There were no score 3 pattern cases in the study.
"The absence of score 3 lesions may be explained by two main factors," the authors wrote. "Firstly, Itoh's original score was invented for the breast, and lesions in the breast have a considerably different histological pattern -- and therefore RTE pattern -- compared with testicular lesions. Secondly, the elasticity score of 3 was mainly found by Itoh in benign lesions of the breast."
In Itoh's study, score 3 benign nodules were larger than 10 mm, which may be found quite often in the breast, but this doesn't happen in the testicle, where the vast majority of large nodules are nearly always malignant, they explained.
An elasticity score of 4 describes a circumscribed and homogeneously harder nodule than the adjacent tissue and indicates no strain in the entire lesion, which is considered characteristic of malignancy. An elasticity score of 5 shows no strain in the entire lesion and the surrounding area, which indicates infiltration of cancer cells into the interstitial tissues.
A prevalence of score 4 and 5 patterns (only one lesion showed score 5 pattern) were found in 87.5% of the malignant cases.
The Leydig tumors in the study were slightly hyperechoic compared with the surrounding tissue and showed mainly an elastic pattern at RTE. At histology, Leydig tumor consists of polygonal cells with abundant, eosinophilic cytoplasm, solid, sheet-like pattern without interstitial fibrous stroma. The progressive growth of this type of tumor induces sclerohyalinosis of the surrounding glandular tissue detectable as a stiff blue rim at RTE.
"On the basis of the correlation between histology and RTE pattern, there could be a possibility of suspecting different malignant histotypes with noninvasive investigation," the researchers wrote. "This could be useful in planning more conservative surgery in selected cases."
"We suggested introducing a further score value (score 3-inverted) -- never described before -- which corresponds to a specific histological pattern," Goddi said in an interview with AuntMinnieEurope.com.
The RTE appearance for Leydig tumors seems the exact opposite of the known score 3 reference, which is why the researchers suggest an additional score.
"Concerning our next steps, we need to confirm such correspondence through a wider range of samples," Goddi said. "A further goal will be the prolonged follow-up of the testicular nodules defined as benign at RTE, in order to confirm that expectant management in selected cases can be possible and convenient thanks to RTE."
Every doctor at SME-Diagnostica per Immagini Medical Center routinely use RTE to characterize the nodules, but not to identify lesions because that is already possible through B-mode ultrasound. What is missing is the characterization of the nodule as benign or malignant, he said.
"RTE of the testicle doesn't need a long training, therefore [it] can be easily performed by almost every sonographer," he added.



















