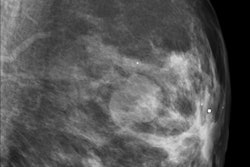
Having a mammogram annually for 15 years and biannually thereafter equates to a radiation-induced risk of breast cancer occurring in one out of every 1,000 women, or one half of 1%, but having a screening mammogram reduces a woman's risk of dying from breast cancer by 50%.
These are among the facts presented by the European Society of Breast Imaging (EUSOBI) in an article summarizing basic information for women about mammography examinations. Published online first 28 October in Insights into Imaging, it explains the difference between a screening and diagnostic mammogram, the best time of the month for premenopausal women to schedule mammograms, and why women are recalled and what procedures are followed next.
EUSOBI also answers five of the most frequently asked questions by patients and explains the classification system terminology of the mammography report. It talks candidly about pain, one of the deterrents for women who are considering the procedure.
Co-authors Dr. Francesco Sardanelli of the Dipartimento di Scienze Medico-Chirugiche's Unità di Radiologia of the Università deli Studi di Milano in Milan, and Dr. Thomas Helbich of the department of radiology of the Medical University of Vienna point out that at least one in every 10 European women are at risk for developing breast cancer in their lifetime. Noting that different radiological and cancer societies in Europe recommend different ages and time intervals at which a woman should have her first mammogram, they suggest that the examination may be performed as early as age 40 or 45.
EUSOBI recommends that, regardless of the starting age, mammograms should be performed on an annual basis to age 50 because tumors generally grow faster in younger women who also tend to have denser breasts. Screening mammography, whether annual or biannual, is recommended from ages 50 to 70, but the authors state that continuing it is acceptable, and patients should request the opinion of a radiologist at that time. Women with a family history of breast cancer occurring before menopause should talk to their radiologist about the frequency of scheduling the examination.
About half of the women who have mammograms find them to be painful, but only 4% of the total say that they are very painful. Pain disappears immediately after the procedure for all but 25% of the women who report pain. The least painful time to have a mammogram is on the seventh to 12th day of a woman's menstrual cycle. This time is also when breasts have their lowest density.
Radiographers should inform women having a mammogram to be alert to unusual breast conditions, such as a nipple discharge, retraction of the skin or nipple, and, of course, a palpable lump. If any of these occur regardless of the frequency of the last mammogram, a woman should contact her doctor.
American women who have a mammogram in Europe and European women who have a mammogram in the U.S. may be confused about the numeric classifications. They are in fact different, and are summarized below:
|