Mammography plus near-infrared breast imaging is slightly -- but not significantly -- more accurate than mammography alone when it comes to detecting breast lesions, German researchers found in a recent European Radiology study.
Radiologists are continually on the lookout for technology that will improve the diagnostic accuracy for detecting breast cancer lesions. Near-infrared (NIR) diffuse optical imaging is a possibility because it has the potential to provide information on the molecular and cellular level that may improve detection and characterization of tumor tissue.
"The economical and compact instrumentation and the absence of ionizing radiation makes NIR imaging very attractive to many investigators," wrote lead researcher Dr. Alexander Poellinger from the department of radiology at Charité Universitätsmedizin Berlin (Eur Radiol, online first, 27 September 2011).
Poellinger and his team investigated the use of a commercially available, NIR imaging system (CTLM, Imaging Diagnostic Systems) as an adjunct to mammography in 276 consecutive patients. Four blinded readers assessed the images to identify a possible increase in diagnostic accuracy compared with mammography alone. There were 72 benign and 52 malignant lesions in the group of 124 lesions for which histologic proof was available.
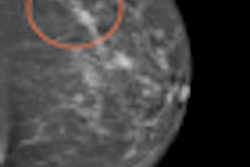
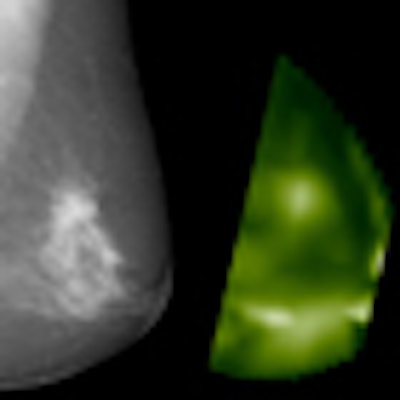
 X-ray mammography (mediolateral-oblique projection) and near-infrared image (CT laser mammography) of a 60-year-old patient with an invasive ductal carcinoma in the left breast. Due to the enhanced hemoglobin concentration, the tumor is shown at high signal on optical mammography compared with the surrounding tissue. Image courtesy of Dr. Alexander Poellinger.
X-ray mammography (mediolateral-oblique projection) and near-infrared image (CT laser mammography) of a 60-year-old patient with an invasive ductal carcinoma in the left breast. Due to the enhanced hemoglobin concentration, the tumor is shown at high signal on optical mammography compared with the surrounding tissue. Image courtesy of Dr. Alexander Poellinger.The benefit of near-infrared breast imaging (NIBI) as an addition to mammography was determined by performing receiver operating characteristics (ROC) analyses for each reader based on BI-RADS categories and level of suspicion (LOS) scores.
For the LOS-based analysis, the combination of mammography and NIBI resulted in a slightly larger area under the curve for all four readers, according to the researchers. The analysis based on BI-RADS categories also demonstrated a slight increase in the area under the curve for three readers for the combination of mammography and NIBI compared with mammography alone. For the fourth reader, the area under the curve was smaller for the combination compared with mammography alone. The researchers found no significant difference between the two methods for either the separate ROC analyses or the multireader-multicase ROC analysis of variance.
"In our study using ROC analysis, we found that the combination of mammography and NIBI performed slightly better than mammography alone in detecting breast cancer; however, the difference in diagnostic accuracy was not significant," the researchers wrote. "Also in dense breasts, no significant difference in diagnostic accuracy was achieved with the adjunct of NIBI."
The authors attributed the results to the following possible reasons:
- Optical mammography is at an early, experimental stage. The readers lack experience.
- Interreader agreement was greater for the interpretation of mammograms compared with the interpretation of NIR breast images.
- The NIBI system used in this study reflects the company's state-of-the-art technology in 2002. Results obtained with more modern equipment would perhaps improve the diagnostic accuracy of NIBI.
- Intrinsic contrast alone (based on hemoglobin) is not sufficient to achieve an adequate specificity using optical mammography. (Contrasts in optical mammography using NIBI arise from differences in the absorption of NIR light, which in turn depends on hemoglobin concentrations in different breast areas.)
Use of contrast medium may overcome this limitation and improve the diagnostic yield of optical mammography, the researchers wrote. In fact, in an interview with AuntMinnieEurope.com, Poellinger said the team is planning on performing further studies on optical mammography using contrast agents.
"Our recent results using indocyanine green and omocianine were very encouraging," he added.