An ambitious new breast screening study, the PROCAS (Predicting Risk of Cancer at Screening) trial, is aiming to not only answer important questions about breast density and cancer development but also evaluate the effectiveness of computer-aided detection (CAD) in the screening of dense breasts. Moreover, it is using the latest genetic tools to improve understanding of disease development in more than 60,000 women.
Data from the first results show nearly 10% of women have a high percentage of dense breast tissue, elevating their risk of developing breast abnormalities. In all, PROCAS will assess 60,000 women screened in Greater Manchester, U.K., 10,000 of whom will be included in a DNA substudy that will examine the genetic implications of women with dense breasts.
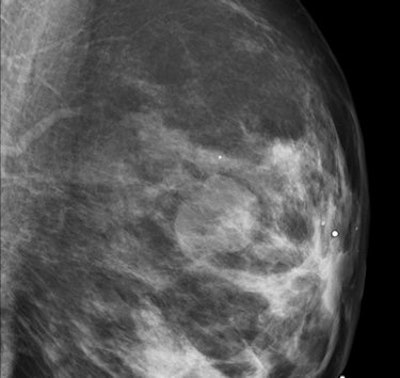
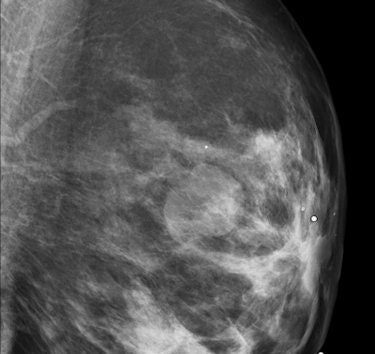 Oblique mediolateral view of the left breast in a 46-year-old woman. A well-delineated lobulated mass can be seen. Ultrasound is needed to classify the lesion as a cyst or a solid mass. All images courtesy of Dr. Luis Pina, University Clinic of Navarra, Spain.
Oblique mediolateral view of the left breast in a 46-year-old woman. A well-delineated lobulated mass can be seen. Ultrasound is needed to classify the lesion as a cyst or a solid mass. All images courtesy of Dr. Luis Pina, University Clinic of Navarra, Spain.Recruitment began in October 2009, and was about halfway complete at the end of September 2011. The study is expected to be completed by October 2012, said PROCAS co-investigator Susan Astley, PhD, in a presentation at the 2011 Computer Assisted Radiology and Surgery (CARS) congress in Berlin.
"We are engaged in a large study which aims to predict women's risk of breast cancer at the time of screening, and, as a result, to explore the possibility of adapting screening according to individual risk," wrote Astley, from the University of Manchester, in an email to AuntMinnieEurope.com.
The association of dense breast tissue with a higher prevalence of disease isn't new, of course. The first studies revealing a relationship between breast density and the risk of carcinogenesis were performed in the 1970s, and the phenomenon has been amply demonstrated in the decades since. Still, important questions -- such as how breast density impacts CAD -- remain unanswered, she said.
"Breast density is an important risk factor for breast cancer, with increased amounts of dense tissue leading to increased risk of cancer," Astley said in her talk at CARS.
The method of determining density is subjective. Traditionally, density has been estimated by visual assessment, usually as the percentage of the area of the breast that is occupied by dense tissue in the mammogram.
The technique is accurate enough, but a problem with previous studies is that they don't examine "differences in imaging, differences in compression, differences in the imaging parameters," she noted. And in this regard, PROCAS is different. It relies on subjective measurements of relative breast density, like previous studies, but asks the reader to rate density on an analog scale of 0% to 100% based on two craniocaudal (CC) views and two mediolateral oblique (MLO) views rather than one each as in some previous studies.
PROCAS uses visual assessment as a baseline, with two independent estimates of percentage density in each image made on visual analog scales. The group is also using a semiautomated thresholding method called Cumulus, an assessment method that has been well-validated against risk, on a selected sample of cases, mostly cancers. A key aim of the study will be evaluating the accuracy of different density-assessment methods.
The problem with density
Dense breast tissue makes care more difficult in at least two ways, Astley explained. First, the presence of dense breast tissue is well-known to increase the risk of carcinogenesis. Fishell, Hanna, and colleagues found a 21% cancer recurrence rate in women with dense breasts (25% to 50% dense tissue) versus 5% in patients with less than 25% dense tissue.
At the same time, dense tissue makes abnormalities more difficult to read, especially on traditional film-screen mammography. The landmark Digital Mammographic Imaging Screening Trial (DMIST) demonstrated better detection of dense-breast abnormalities using full-field digital mammography (area under the curve [AUC] 0.78 ± 0.02) versus film-screen mammography (AUC 0.68 ± 0.03).
"Dense breasts can mask cancer that's there, reducing contrast," Astley said. "Its effect on CAD isn't clear-cut; there is conflicting evidence in the literature. Some say it tends to reduce the performance of CAD, while other work shows no effect."
The PROCAS process
PROCAS aims to predict breast cancer risk in women undergoing routine screening in the U.K.'s National Health Service (NHS) Breast Screening Programme, "predicting their risk based on mammography and genetic material and a questionnaire that asks for risk information," Astley said.
The study will investigate whether screening intervals can be adapted according to risk. Other aims include validation of density methods and determination of the best way to measure breast density -- volume or area, specific views, and percentages of fat and glandular tissue. The investigators will look at density patterns, locations, and differences, both temporal and left versus right, and finally prevention measures.
"There are different standards as to what is high risk," she said. "Is it over 50% or 75%? There are different measurements and differences in views used to assess density. Some studies look at volume of dense tissue and some look at the percentage of dense tissue as a whole."
Finally, the investigators will explore the relationship between breast density and other risk factors such as alcohol consumption and weight, incorporating breast cancer and breast density single-nucleotide polymorphisms (SNPs) in the Tyrer-Cuzick risk prediction model. They will compare different risk-prediction models in general, and investigate the utility of different density measurement methods for risk prediction.
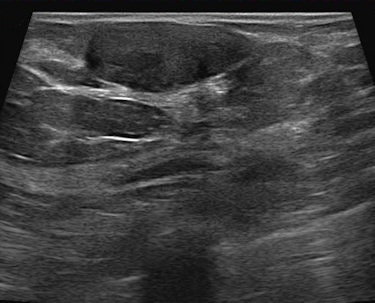 Ultrasound confirms the lesion as a solid homogeneous mass, parallel to the skin. These features suggest a fibroadenoma, but this lesion meets the criteria of the BI-RADS 3 category. Follow-up showed no changes over two years.
Ultrasound confirms the lesion as a solid homogeneous mass, parallel to the skin. These features suggest a fibroadenoma, but this lesion meets the criteria of the BI-RADS 3 category. Follow-up showed no changes over two years.Each PROCAS participant fills out a two-page questionnaire that includes questions about lifestyle, family history, weight, height, ethnicity, reproductive history, and other questions related to risk factors, with genetic material being taken from about one-sixth of the women. All participants are undergoing routine screening, of course, so their mammograms will be analyzed and incorporated with other findings. Finally, women who are determined to be at high risk -- along with some low-risk participants -- are offered a consultation to receive advice, and, when appropriate, therapeutic intervention, Astley said.
High-risk, and some low-risk, participants receive preliminary risk information based on breast density and the Tyrer-Cuzick risk estimation model of breast cancer risk factors.
A second mammography screening is scheduled three years after baseline -- the normal interval in the U.K., she said. "Then we combine the DNA and questionnaire information to assess the risk in detail, and by that time we will have modified the Tyrer-Cuzick model to take these things into account," she said. "All women in the study, if they want, can receive this information."
Some high-risk participants (> 60% dense breast tissue; > 8% 10-year risk per Tyrer-Cuzick) and very low-risk women (<20% dense tissue; < 1.5% 10-year risk) receive face-to-face or telephone consultation with a clinician. As of late June, 129 women had received feedback about their risk, she said, of which 71 were set to be rescreened in 18 months. Other participants have joined additional studies.
"The reason we included low-risk women is that we didn't want word going around that if you get invited for a risk assessment it means you're high-risk," Astley said.
Exploring measurement methods
Relative methods of density assessment suffers from an important drawback -- women who lose weight lose fat from their breasts, leading to an increase in percentage density -- a result that is at odds with the known relationship between excess weight and cancer risk. It is particularly a problem in the screening population where womens' weight may vary considerably over a period of months, Astley said.
To correct for the phenomenon, "we are also measuring the actual amount of dense tissue in the breasts," Astley explained. "In film mammograms, we are using a method we developed ourselves, where a calibrated step wedge is imaged alongside the breast. In digital images, we are evaluating commercial software."
To date, the great majority of the group's digital images have been analyzed with Quantra software (Hologic), which calculates the volumes of fat and gland in the breast, and can also output a relative measure (percentage density by volume). The method is model-based, using knowledge of the imaging parameters and physical process to calculate these values from the digital image data.
"We are also beginning to investigate Volpara (Matakina Technology)," another model-based approach, Astley said. "Volumetric methods tend to give lower relative values [lower percentage density] than area-based methods, because they take into account the three-dimensional nature of the breast. Unlike visual assessment techniques, they are not operator-dependent. Should our study indicate that risk-adapted screening would be an appropriate way forward, automatic analysis will be essential."
Early data
As of June, about 25% of the more than 42,000 women (ages 37-74 years) invited for screening both attended routine screening and consented to enter the trial, according to Astley, and 94% said they wanted to be told about their individual risk. About 10,000 women had been included in the DNA substudy. It has been more difficult to recruit poorer women and Asians, she said.
In results analyzed so far, the percent dense area (per visual assessment score [VAS] ranged from 0.625% to 97.25% [mean 29.16%, median 25.38%]). VAS is one of three density-assessment methods (in addition to Cumulus and step wedge) employed for each full-field digital mammography scan.
Also, as of late June, 8.32% of women screened had density of greater than 60%, she said. The 10-year risk of cancer from the Tyrer-Cuzick model ranged from 0.76% to 24% (median 2.65%).
SNPs testing on the first 421 saliva DNA samples gave a wide range of relative risks: the mean 10-year predicted risk of 2.7%, range 0.7% to 11.88%.
Importantly, the investigators have noted that the inclusion of DNA information leads to a wider spread of risk than the Tyrer-Cuzick model alone, particularly at the lower-risk end of the risk scale, Astley said.



















