What prompts radiologists to provide intermediate mammograms should be characterized so they can give useful recommendations and minimize the adverse effects of the procedure, Spanish researchers have found in an online first article published in European Radiology.
In Spain, breast cancer screening is offered to all women in the target population, but some differences among regions could lead to variations in the results of these national screening programs. In general, the interval between screening rounds is two years, but in certain circumstances an earlier recall is recommended (it generally takes place 12 months after the last screening mammogram).
The effects of these intermediate mammograms are potentially positive, but their effectiveness in reducing mortality and improving the risk/benefit ratio is unclear, according to Nieves Ascunce from the Navarra Breast Cancer Screening Program, Public Health Institute in Pamplona, Spain (Eur Radiol, 8 September 2011).
Ascunce and her team analyzed the use of intermediate mammograms: their frequency, the personal- or protocol-related variables leading to their indication, their effect on the risk of a false-positive result in the screening episode in which they are performed, and their effect on the detection of malignant tumors.
Of more than 3.4 million mammograms, 3.36% were intermediate mammograms. Intermediate mammograms should be indicated after mammograms are included in category 3 of BI-RADS, and only after complete evaluation of the screening test and any additional procedures -- otherwise diagnosis of any malignancy could be delayed, according to the researchers. "Under these circumstances, intermediate mammograms demonstrating the stability of the lesion could reduce the number of biopsies," they wrote. "In our study, slightly more than half of intermediate mammograms were directly indicated by the screening test."
The researchers found the factors associated with the use of intermediate mammograms were age, initial screening, previous invasive tests, a familial history of breast cancer, and use of hormone replacement therapy.
Early rescreens were recommended three times more frequently in women undergoing their first screen than in those undergoing subsequent screens, according to Ascunce. This finding is in agreement with those of U.S. study reporting intermediate mammograms in 5% of initial screenings, decreasing to 2% in subsequent screenings, the authors wrote.
The availability of previous mammograms also reduced the frequency of early rescreens; this procedure was more frequent in the initial screen, when no previous mammograms are usually available, according to the authors.
Independent of the screening type, the older the woman, the less frequent the recommendation for an intermediate mammogram, which is probably linked to a change in breast density, a factor not evaluated in the study.
The probability of a false-positive result was 13.74%, almost double that in episodes without intermediate mammograms (6.02%). However, in young women with previous invasive procedures, a familial history of breast cancer, or hormone replacement therapy use who were undergoing their initial screen, the probability was lower when intermediate mammograms were performed, according to the researchers. Lastly, intermediate mammograms always increased malignant tumor detection rate, mainly in women without risk factors.
"The probability of undergoing an intermediate mammogram depends on the presence of risk factors," the authors wrote. "Unsurprisingly, therefore, women undergoing intermediate mammograms are at higher risk of cancer."
However, even after adjusting for those variables, the malignancy detection rate was increased by intermediate mammograms. "This increase was even higher in women without associated risk factors, although this finding could have been due to the presence of other risk factors not evaluated in this study," the authors wrote. "The increased detection rate should not necessarily be viewed as a beneficial effect per se, unless a consequent decrease in mortality is demonstrated."
Limitations of the study included lack of data and information on important factors such as the availability of previous mammograms, breast density, the type of mammographic abnormality, etc. Another is the lack of information on radiologists' experience, which could be a major influence in the recommendation of intermediate mammogram follow-up and the false-positive rate.
"Screening programs should follow protocols that guarantee their quality, and intermediate mammograms should only be recommended if they improve women's health," the researchers wrote. "In our study, early rescreens were performed more frequently than recommended, increasing the rate of false-positive results. Intermediate mammograms avoid the use of additional tests with a negative result only in specific groups of women -- those undergoing their initial screen, younger women (aged 45-49 or 50-54 years), and those with risk factors ... but whether this effect significantly reduces mortality remains to be determined."
Intermediate mammograms should be performed as sparingly as possible, the researchers concluded. They recommend the following:
- Original and continuous training of reading radiologists should be established so they use standard criteria.
- Previous mammograms should be available whenever possible.
- Intermediate mammograms should be recommended only when images of doubtful significance have been confirmed and only after additional evaluation, and should not be recommended based solely on the presence of personal risk factors such as a family history of breast cancer.
- The factors determining the recommendation for intermediate mammograms should be better characterized so reading radiologists can standardize their indications.
- Women should also be informed of these results, the protocols applying intermediate mammograms according to risk, and the potential benefits and drawbacks of this practice.
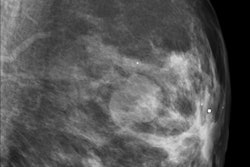
Note: The image on the home page is a digital breast image, tomosynthesis slice. Image courtesy of Siemens Healthcare.