A key benefit of 3-tesla MRI is that it enables doctors to visualize and recognize ligaments in the knee and the smaller joints, such as the posterolateral corner, according to Dr. Edwin Oei, PhD, a musculoskeletal radiologist and primary investigator of the Musculoskeletal Imaging Research Group at Erasmus Medical Center in Rotterdam, the Netherlands.
"If not managed correctly, posterolateral corner injuries can cause chronic pain and instability of the knee, and can also lead to anterior and posterior cruciate ligament reconstruction failure and secondary osteoarthritis," he told delegates at the International Symposium on State-of-the-Art Imaging (iSi 2011), held last week in Bordeaux, France.
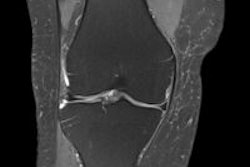
Associated with injuries to the cruciates, menisci, bone, and soft tissue, this disorder still remains easy to overlook, particularly on 1.5-tesla machines. Besides the anatomical complexity, confusion about the posterolateral corner is compounded by controversies and inconsistent reports in the literature, and radiologists often don't look for it, despite its seriousness.
"Because it is associated with easily recognizable ligament tears, many radiologists are satisfied when they see these first lesions and stop reading the image," Oei noted. "Yet from a radiological perspective, posterolateral corner is more important to recognize than those more obvious lesions, and we have a role in attracting the orthopedic surgeon to it."
He outlined other common trauma mechanisms and injury patterns, and demonstrated vastly improved visualization with 3 tesla of both ligamentous lesions and microfractures in the bone. In addition, he pointed to the emergence of new techniques to assess joints opening up new possibilities for disease and injury management.
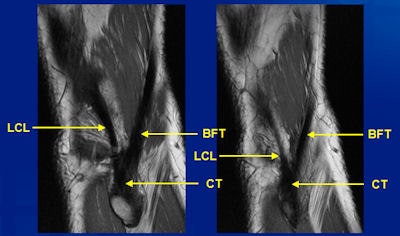 3-tesla MRI clearly shows detailed anatomy of the biceps femoris tendon, the conjoint tendon, and the lateral (fibular) collateral ligament in the posterolateral corner. All images courtesy of Dr. Edwin Oei.
3-tesla MRI clearly shows detailed anatomy of the biceps femoris tendon, the conjoint tendon, and the lateral (fibular) collateral ligament in the posterolateral corner. All images courtesy of Dr. Edwin Oei."It's not always true that with better image quality, one also necessarily achieves a better diagnosis. For many patients, 3T isn't necessary, but in others, doctors would miss a subtle ligamentous abnormality or cartilage lesion with only 1.5T," said Oei, adding that larger patient groups were needed to prospectively assess what added value higher field strength brings and to determine the criteria needed to stream patients accordingly.
At Erasmus, an upgrade for one of the MRI systems has meant that most musculoskeletal patients are now routinely imaged at 3 tesla. The result has been not only clearer images but also clearer reports for referring physicians, and radiologists are now more confident about excluding abnormalities based on image quality. In addition, Oei noted the potential of sensitive imaging technology, combined with quantitative imaging techniques for cartilage, to target early treatments aimed at modifying disease progress and revolutionize the management of osteoarthritis patients.
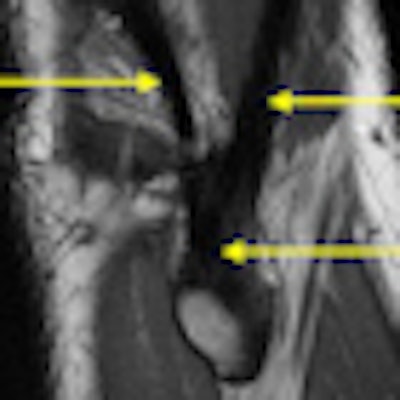
 Dr. Edwin Oei receives treatment after a direct injury to the knee caused by a fall during a football game. Knowing how a patient sustains injury gives radiologists an advance warning about what injuries to look for.
Dr. Edwin Oei receives treatment after a direct injury to the knee caused by a fall during a football game. Knowing how a patient sustains injury gives radiologists an advance warning about what injuries to look for.
"Rather than morphological imaging, which is highly subjective and only looks at the end-stage disease process, we are moving toward numerical assessment of hip and knee cartilage composition. Only then can you follow patient groups after treatment," he said. "The Holy Grail in musculoskeletal radiology is to have a stable reproducible and sensitive outcome measurement that you can use on one patient at different time points, and we are working hard to achieve that."
Oei pointed to the benefits of prior knowledge regarding "pattern recognition" of soft-tissue lesions and bone contusion based on trauma mechanism, such as dashboard, clip, or pivot shift, and associated injuries.
"If you know how a patient sustained a knee injury, you can expect images before you see them, and then you can scrutinize the correct areas in detail. That is a more effective method of diagnosis than not knowing anything and interpreting an MRI from scratch," Oei said. "In addition, radiologists should be familiar with the posterolateral corner."