An upright MRI technique makes it possible to recognize the stability of a meniscal tear and avoid potential damage from arthroscopic investigations, leading to more rapid recovery from injury, according to Italian researchers.
"This new approach to meniscal pathologies helps in the diagnostic and therapeutic care of patients," noted Dr. Antonio Barile from the department of radiology at the University of L'Aquila, San Salvatore Hospital. "It shows both meniscal tear stability and a latent instability, making it possible to correctly guide the orthopedic surgeon toward a conservative treatment, meniscal repair, or rather toward a partial meniscectomy."
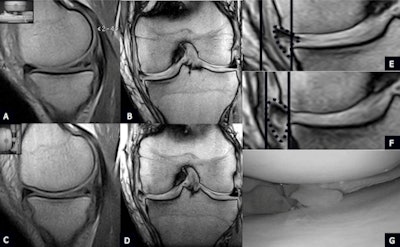 |
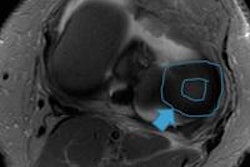
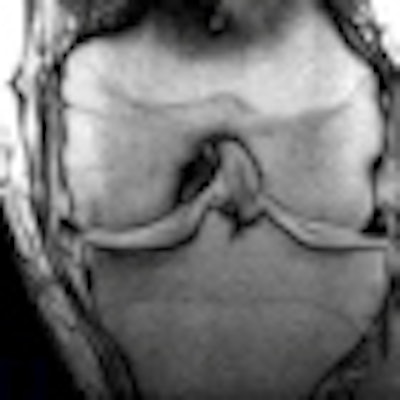
| Unstable degeneration (type 3 lesion) of the medial meniscus. Type 3 degeneration tear of the medial meniscus well-depicted on sagittal PD-W (A) and coronal GE-W (B) scan planes in the supine position. (C) Sagittal scan plane PD-W in the orthostatic position shows fragmentation of the meniscus. (D) Coronal weight-bearing GE-W suggests an unstable lesion well-depicting a lateral shift of the meniscus: See lines in (E) supine and (F) upright. (G) Arthroscopy confirms unstable and fragmented type 3 degenerative tear of the medial meniscus. All images courtesy of Dr. Antonio Barile. |
Barile and his colleagues sought to assess the role of dedicated low-field standard and weight-bearing MRI in the evaluation of stable or unstable tears of medial meniscus in comparison with arthroscopy. They studied knee MRI examinations performed with a 1.5-tesla MRI scanner (Signa Horizon, GE Healthcare) from July 2010 to August 2011, and reported their findings in an article in press published online in the European Journal of Radiology (30 November 2012).
All examinations were performed using a dedicated coil. Based on the MRI diagnoses, the patients were divided into two groups. The first included 12 male and eight female patients, whose age ranged from 18 to 52 years (mean, 36.5). They presented with a clinical diagnosis of anterior knee pain with neither prior history of trauma nor lesions and/or ligament and meniscus instability. The second group included 33 male and 24 female patients, ranging in age from 18 to 54 (mean, 37.5), who presented with a clinical suspicion of medial meniscus injury, previously diagnosed by an orthopedic surgeon and then documented by MRI.
The authors retrospectively reviewed and analyzed 20 MRI exams of normal knees and 57 MRI exams of knees with clinical evidence of tears of the medial meniscus. In the same session, after conventional 1.5-tesla and dedicated 0.25-tesla supine MRI examination, the patients underwent a weight-bearing examination with the same dedicated MRI unit. In all cases, sagittal and coronal proton-density weighting were used. All patients underwent arthroscopy 18 to 25 days after the weight-bearing MRI.
 |
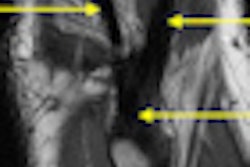
| Unstable longitudinal traumatic tear of the medial meniscus posterior horn. (A) Sagittal scan plane PD-W in the supine position shows a longitudinal tear of the posterior horn of the medial meniscus. (B) Sagittal scan plane PD-W in the weight-bearing position shows the increased intrameniscal extension of the lesion on the axial plane: See magnification from image B in C (arrow). (D) Arthroscopy confirms unstable traumatic longitudinal tear of the medial meniscus posterior horn. |
In the first group, no statistically significant anatomical modifications of shape, intensity, and position of the medial meniscus were observed between standard 1.5-tesla, dedicated supine, and upright MRI. In group A, the images acquired in the supine position (dedicated and 1.5-tesla MRI) documented in 21 cases a traumatic tear (group 2A) and in 36 cases a degenerative tear (group 2B).
"After an 82° table rotation, MRI examinations allowed evaluation of the physiological variations of the signal under physiological load, as well as of the medial meniscal position and morphology. Morphology, intrameniscal signal and measurements of the grade of medial meniscal extrusion, evaluated on both sagittal and coronal planes, did not show statistically significant differences," they wrote.
In group 2A, weight-bearing MRI showed the presence of an unstable tear in only 19 out of 36 cases. In group 2B, weight-bearing MRI showed this in only nine out of 21 cases. Arthroscopy confirmed the weight-bearing MRI diagnosis in all cases.
This new approach to meniscus pathology makes an important contribution to improving patient management in an area in which MRI has not played a key role so far, according to the authors.
In spite of the excellent results, further studies are needed on a larger series of patients, possibly in a multicentric study, they stated. Currently, Barile's group is working on femoropatellar instability using dedicated weight-bearing MRI. He reports that their initial results are very satisfying.