Take a closer look at the meniscus when imaging and avoid over- or undercalling common meniscus pathologies. That's the advice of Dr. Gustav Andreisek, head of musculoskeletal and MR imaging at the University Hospital of Zurich, Switzerland. In particular, portions of the meniscus, such as the roots or the ligamentous attachments of the meniscus to the capsule, are usually missed during reporting, he explained.
Abnormalities of the meniscus are common, especially in the elderly population. Depending on a patient's age, meniscal tears have been reported to occur in about one-third to one-half of patients complaining of knee problems. Andreisek pointed out that a distinction needs to be made between meniscal tears related to an acute trauma and tears secondary to degeneration. Among those tears related to sports injuries, the most frequent causes include skiing, football, field hockey, and squash.
At today's ECR 2015 refresher course, he discussed some of the technical issues relating to imaging protocols in order to acquire high-quality images of the meniscus; the standard anatomy of the menisci, including the roots and their ligamentous attachments; and clinical cases aimed at illustrating the most common pitfalls in the pre- and postoperative knee, with advice on how to avoid them.
First, Andreisek highlighted the importance of using an appropriate imaging protocol. "Most frequently coronal and sagittal fast spin-echo sequences with a high resolution and a good contrast are used," he began. "Second, it is important to really look at every portion of the meniscus and this includes the meniscus roots. Often, radiologists only look at the anterior and posterior horn and the intermediate portions, but it is also very important to have a close look at the roots of the meniscus. Missing a tear may result in instability."
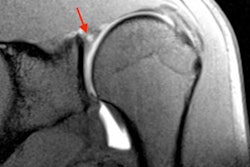
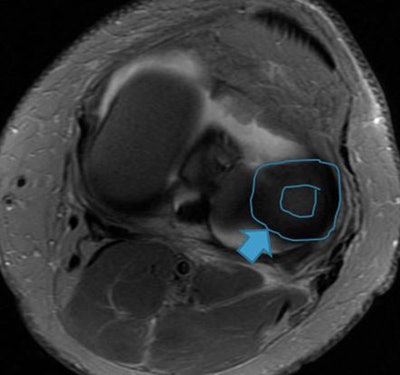 Image shows lateral discoid meniscus. Instead of the normal meniscal shape (triangular in cross-section and C-shaped), it appears in the shape of a disk. Image courtesy of Dr. Gustav Andreisek.
Image shows lateral discoid meniscus. Instead of the normal meniscal shape (triangular in cross-section and C-shaped), it appears in the shape of a disk. Image courtesy of Dr. Gustav Andreisek.He also pointed out the importance of radiologists using clear language accompanied by a precise description in addition to rating systems to describe meniscus abnormalities. "This is more likely useful for the clinician than any grading system."
Asymptomatic meniscal tears also are worth noting. A landmark paper by Zanetti et al (American Journal of Roentgenology, September 2003, Vol. 181:3, pp. 635-641) showed that several meniscal abnormalities are frequently found in asymptomatic patients. The authors evaluated the contralateral healthy knee in 100 patients who underwent MRI of a symptomatic knee. It was shown that especially horizontal and oblique meniscus tears are very frequent in the asymptomatic knees, whereas radial, vertical complex, and displaced tears are likely more relevant and associated with pain and symptoms.
Andreisek added that it was very likely that those abnormalities/tears do not have any clinical relevance. "These abnormalities need to be considered during image interpretation."
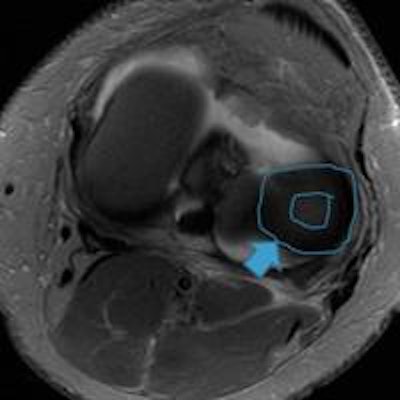
Continuing the theme of diagnostic and therapeutic challenges, Dr. Simone Waldt, associate professor of radiology at the Technical University of Munich, Germany, raised the subject of patellofemoral instability and osteochondral lesions in her talk, during the same session. In the refresher course, she discussed standardized imaging methods in order to assess abnormalities that are predisposing for patellofemoral instability, for example, trochlear dysplasia, patella alta, tibial tuberosity-trochlear groove (TT-TG) distance, rotational deformities of the lower limb, and patellar tilt. Her talk aimed to improve the reporting of osteochondral injuries and patellofemoral abnormalities.
She highlighted that with MRI the characteristic pattern of acute injuries and the severity of lesions can be assessed accurately, and in the diagnosis of acute and often overlooked lateral patellar dislocation, the modality provides critical information.
"Acute and often overlooked lateral patellar dislocation can be established with magnetic resonance imaging because of its characteristic pattern of injury. In particular, the integrity of the MPFL [medial patellofemoral ligament] should be assessed carefully. This ligament is the most important passive stabilizer of the patellofemoral joint. The MPFL should be assessed on transverse images," she noted.
Waldt highlighted that treatment decisions with respect to osteochondral lesions (surface lesions that have a traumatic etiology and involve both the cartilage and subchondral bone), required that the following key questions should be answered by means of imaging: the integrity of the cartilage over the lesion, the stability of the (osteo)chondral fragment, and the integrity of the cartilage of the opposite side of the joint.
She also discussed diagnosis and therapeutic options for chronic instability. "It is extremely important to consider that the cause is usually multifactorial, so that therapeutically a unilateral approach often does not lead to improvement in symptoms," she highlighted. "Important factors to consider are trochlear dysplasia, patella alta, TT-TG distance, rotational deformities of the lower limb, and patellar tilt."
A typical pitfall in the diagnosis and treatment of chronic instability is that not all relevant etiological factors are considered during preoperative planning. "One could suggest the following diagnostic procedures as guidelines in the preoperative assessment: radiographs in two planes, a CT to assess potential rotational deformities and the TT-TG distance, and MRI in the acute setting," she concluded.
Originally published in ECR Today on 6 March 2015.
Copyright © 2015 European Society of Radiology