With the help of contrast-enhanced (CE) MRI, British researchers have found that patients with breast cancer who have higher levels of vascularization after two cycles of neoadjuvant chemotherapy are likely to have lower survival rates, according to a study in the July issue of Radiology.
Contrast-enhanced MRI's ability to measure vascularity after treatment may serve as a way to predict disease outcome in patients undergoing chemotherapy. Patients whose tumors show greater vascularity after chemotherapy as a result of poor response to treatment could have their therapies changed to better address tumor vasculature.
The lead author of the study was Dr. Sonia Li from Mount Vernon Cancer Centre in Middlesex, U.K. (Radiology, July 2011, Vol. 260:1, pp. 68-78).
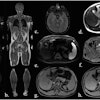
Researchers recruited 73 female patients with breast cancer to undergo contrast-enhanced MRI before and after two cycles of chemotherapy between January 2001 and September 2008 as part of two sequential prospective studies. The study excluded patients who were pregnant or had any contraindications to MRI.
MRI was performed on 62 patients before and 58 patients after the two cycles of chemotherapy. Among the 73 patients, three were found to have metastatic disease after enrollment, eight were unable to undergo their first MRI scan, and four did not receive a second MRI exam.
The median age at diagnosis was 45 years, ranging from 22 to 70 years, and the median tumor size for the group was 50 mm, ranging from 10 to 100 mm. The median number of chemotherapy cycles was six, ranging from two to eight cycles.
After chemotherapy, the patients received additional treatment with surgery, postoperative external-beam radiation therapy to the breast or chest wall, endocrine therapy if a patient had positive hormone receptor status, and trastuzumab if a patient had positive HER2 status.
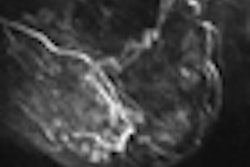
MRI scans were conducted on a 1.5-tesla scanner (Symphony, Siemens Healthcare) with a dedicated bilateral breast coil. The researchers acquired initial diagnostic T1- and T2-weighted images through the center of the tumor, followed by proton density-weighted gradient-echo images of four sections: three through the tumor and one through the contralateral normal breast.
Gadopentetate dimeglumine (Magnevist, Bayer HealthCare Pharmaceuticals) was injected intravenously at 0.1 mmol/kg of body weight for both T1- and T2-weighted MRI scans. Forty sets of dynamic T1-weighted images and 60 sets of T2-weighted images were then obtained.
Disease-free survival was defined as the time from radical treatment to the date of first breast cancer recurrence, date of death, the last known date of no disease, or the date of the most recent follow-up. Overall survival was calculated as the time of the first diagnosis of breast cancer to the date of death, the last known date of a patient being alive, or the date of most recent follow-up.
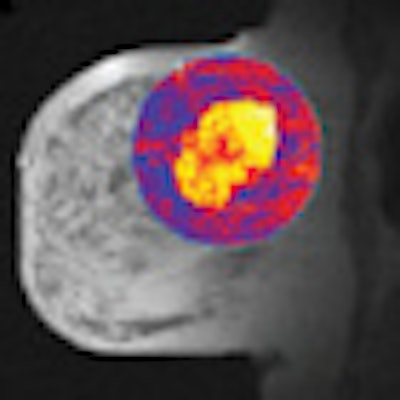
In addition, the researchers used the kinetic MRI parameter inflow transfer constant (Ktrans) to measure vascularity. Ktrans calculates the transfer of contrast between blood plasma and the tumor.
Chemotherapy response
The final analysis showed that 38 (61%) of the 62 patients showed a pathologic response to chemotherapy and were classified as pathologic responders. The remaining 24 patients (39%) did not respond to treatment and were deemed to be nonresponders.
Of the 62 patients, 47 (76%) exhibited a partial or complete clinical response and were considered clinical responders. The remaining 15 patients (24%) were classified as nonresponders due to the stable or progressive stage of their breast cancer. Ten women (16%) achieved a complete pathologic response to chemotherapy, while 52 (84%) did not.
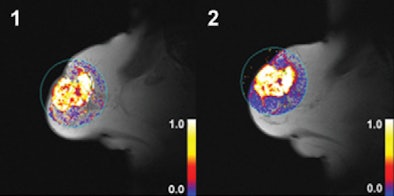 |
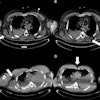
| Dynamic T1-weighted MR images of a 60-mm grade 2 breast carcinoma in the right breast of a 70-year-old woman whose disease relapsed 38.8 months after diagnosis. The patient died 47.2 months after initial radical treatment. Her tumor displayed high values for Ktrans after two cycles of chemotherapy. (1) Ktrans before treatment; (2) Ktrans after treatment. Images courtesy of Radiology. |
The researchers also determined that the median follow-up time for disease-free survival was 43.9 months, ranging from 0.3 to 99.2 months. The median follow-up time for overall survival was 60.3 months, ranging from 10.9 to 104.1 months.
Among the patients, there were 28 cases of recurrence: 26 patients had distant metastases, two of whom also had local recurrence, and two patients had local recurrence only.
Twenty-eight patients underwent breast-conserving surgery, and 30 received a total mastectomy. Instead of surgery, four patients received external-beam radiation therapy as follow-up. There were 20 deaths within the patient population, all related to breast cancer.
The researchers' univariate analysis found that the type of surgery performed and higher post-treatment Ktrans were among the significant predictors of worse disease-free survival. The same analysis concluded that clinical tumor stage and type of surgery performed were among the significant predictors of overall survival.
Patients with breast cancer "exhibiting higher levels of vascularization after two cycles of [neoadjuvant chemotherapy] experience worse disease-free and overall survival," and contrast-enhanced MRI measures of vascularity after treatment "may act as predictors of disease outcome in patients undergoing [neoadjuvant chemotherapy]," Li and colleagues concluded.
The authors cited limitations of the study such as the relatively small number of enrolled patients, adding that the results "should be interpreted with caution" and "further exploration with larger studies is warranted."