Mammography and ultrasound are useful front-line imaging tools for tackling the challenging medical issue of unexplained nipple discharge, but Italian researchers emphasize that breast MRI can find additional cancers, not recognized or occult when conventional imaging is used.
An underlying malignant lesion can be found in up to 21% of cases of patients with nipple discharge, according to Dr. Michele Lorenzon, from the Institute of Radiology, Azienda Ospedaliero-Universitaria Santa Maria della Misericordia, in Udine, Italy, writing in the May edition of European Radiology (Vol. 21:5, pp. 899-907).
For these patients, a complete clinical history and physical examination, as well as mammography and ultrasound, are of primary importance. Cytological analysis of secretion material also is essential, but negative or benign findings cannot exclude an underlying malignancy. Galactography has some invasiveness but is time-consuming and often inconclusive. Breast MRI's importance relies on its high sensitivity for papillomas and for intraductal and invasive carcinomas, he noted.
"Our experience is concordant with the previously published literature: Breast MRI was really useful for several patients with nipple discharge leading to a diagnosis that would have been achieved later with conventional imaging, or that would have not been achieved at all," Lorenzon commented. "So far, the follow-up of the patients with benign breast MRI findings included in our study is negative for malignancies."
The researchers retrospectively evaluated 38 women with nipple discharge who underwent mammography, ultrasound, and 1.5-tesla contrast-enhanced MRI (CE-MRI) between March 2007 and July 2009.
They found a total of five of 38 malignancies (13.2%; three invasive, two intraductal, four ipsilateral, and one contralateral to nipple discharge) and 14 of 38 high-risk lesions (36.8%; 11 intraductal papillomas, one papilloma with lobular carcinoma in situ, one sclerosing papilloma, and one atypical intraductal hyperplasia, all ipsilateral).
The chart belows shows the number of cancers and high-risk lesions each modality detected, as well as the overall sensitivity and specificity for each.
|
Three of the five cancers (one invasive, one in situ, and one invasive contralateral) and two of the 14 high-risk lesions were detected by CE-MRI only. One of the 14 high-risk lesions was detected by ultrasound only.
Compared with mammography and ultrasound, CE-MRI showed statistically significantly higher overall sensitivity values (p < 0.0001, p = 0.042, respectively).
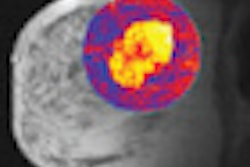
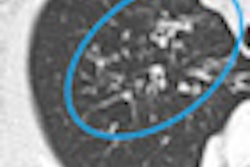
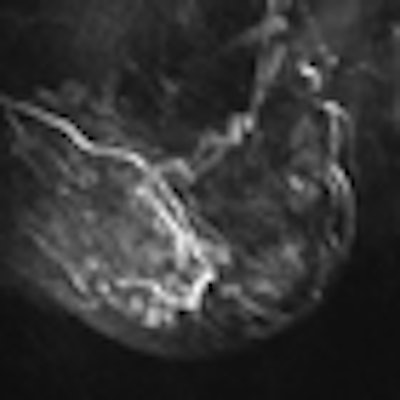
 Patient presented with spontaneous, brown, right nipple discharge that had lasted for one year. Personal history, physical examination, mammography and ultrasound (images above) revealed only benign findings (bilateral fibroadenomas and duct ectasia in the outer quadrants of the right breast). During cytological analysis of secretion material, a papillary lesion without atypia was found. All images courtesy of Dr. Michele Lorenzon.
Patient presented with spontaneous, brown, right nipple discharge that had lasted for one year. Personal history, physical examination, mammography and ultrasound (images above) revealed only benign findings (bilateral fibroadenomas and duct ectasia in the outer quadrants of the right breast). During cytological analysis of secretion material, a papillary lesion without atypia was found. All images courtesy of Dr. Michele Lorenzon.Based on these results and on published papers, in cases of suspicious nipple discharge with inconclusive conventional imaging, Lorenzon and his colleagues now perform breast MRI instead of galactography. However, they are collecting additional cases of patients with suspicious nipple discharge undergoing breast MRI.
Breast MRI can be considered a diagnostic leader in patients with unexplained nipple discharge because malignant and high-risk lesions missed at conventional imaging can be found, they concluded. Ultrasound is complementary to breast MRI and can be considered an excellent adjunct in the case of suspicious findings. Ultrasound has very high sensitivity when focused on lesions found at breast MRI; bilateral, whole-breast ultrasound examination, without knowledge of breast MRI findings, has lower sensitivity.
 Breast MRI showed a suspicious non-mass-like enhancement in the inferior-outer quadrant of the right breast, occupying approximately 50 mm in the axial plane. The final pathological diagnosis was papillary carcinoma with extensive intraductal carcinoma.
Breast MRI showed a suspicious non-mass-like enhancement in the inferior-outer quadrant of the right breast, occupying approximately 50 mm in the axial plane. The final pathological diagnosis was papillary carcinoma with extensive intraductal carcinoma.