German researchers have found that the fusion of 3-tesla MR images with x-ray mammograms can help to accelerate clinical workflow and boost diagnostic accuracy.
The semiautomatic image registration of x-ray mammography and high-field MRI is both feasible and beneficial, noted lead author Dr. Matthias Dietzel, from the Institute of Diagnostic and Interventional Radiology at Friedrich-Schiller-University Jena, in a pilot study described in the European Journal of Radiology.
"For the time being, we have made no changes to our routine workup," he told AuntMinnieEurope.com. "After thorough clinical evaluation of the system, routine use of the software seems to be promising. However, more clinical data are necessary. We are working on this!"
Both x-ray mammography and MR mammography (MR-M) have limitations. The latter technique has the highest sensitivity for detecting breast cancer, but doubts remain over its availability, cost-effectiveness, and specificity. On the other hand, x-ray mammography is relatively cheap and broadly available. It produces good diagnostic accuracy and can visualize microcalcifications, but its sensitivity in dense breasts is limited, especially in younger women, Dietzel explained.
Due to their different physical basis, conventional and MR-M are likely to provide complementary diagnostic information, so both modalities are usually read in combination for a definite diagnosis, he continued. But because the former is a classical 2D method and the latter provides 3D volumes, exact topographic correlation of suspect findings can be difficult and time-consuming, requiring a high level of training.
Medical image registration software can match different modalities, as in the case of PET/CT. The authors think that no report of breast registration at 3 tesla has been published to date, and this prompted them to conduct a pilot study. MR-M was acquired on a high-field clinical scanner at 3 tesla (Magnetom Trio, Siemens Healthcare), while x-ray mammography was performed on a full-field digital system (Selenia, Hologic). They enrolled seven patients with clearly delineable lesions with a diameter greater than 10 mm (Eur J Radiol, 13 May 2011).
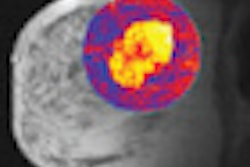
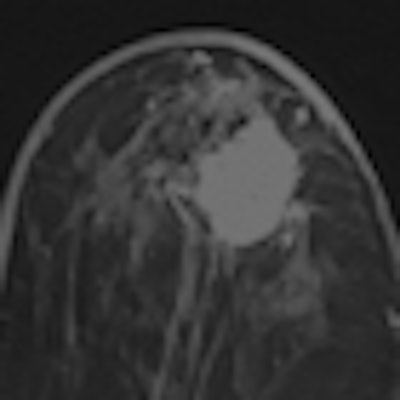
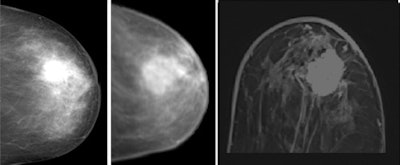 Clinical example of image registration of conventional mammography with high-field MR mammography at 3 tesla. Left, craniocaudal conventional mammography. Middle, virtual craniocaudal mammography. The latter was calculated by the registration software based on the 3D MR mammography dataset. In the image on the right, an exemplary axial view is shown, covering the central part of the advanced enhancing mass (first minute after Gd-DTPA). Histological verification after imaging revealed invasive ductal carcinoma. Images courtesy of Dr. Matthias Dietzel.
Clinical example of image registration of conventional mammography with high-field MR mammography at 3 tesla. Left, craniocaudal conventional mammography. Middle, virtual craniocaudal mammography. The latter was calculated by the registration software based on the 3D MR mammography dataset. In the image on the right, an exemplary axial view is shown, covering the central part of the advanced enhancing mass (first minute after Gd-DTPA). Histological verification after imaging revealed invasive ductal carcinoma. Images courtesy of Dr. Matthias Dietzel.The team matched x-ray mammography and MR-M using a dedicated image registration algorithm that allows semiautomatic nonlinear deformation of MR-M, based on finite-element modeling. To identify registration errors, a virtual craniocaudal 2D mammogram was calculated by the in-house software from MR-M (with and without gadodiamide [Gd]) and matched with corresponding x-ray mammograms. To quantify registration errors, the geometric center of the lesions in the virtual versus conventional mammogram was subtracted. The robustness of registration was quantified by registration of x-ray mammograms to both MR mammograms with and without gadodiamide.
Image registration was performed successfully for all patients. The overall registration error was 8.2 mm (1 minute after Gd; confidence intervaI [CI]: 2.0-14.4 mm, standard deviation [SD]: 6.7 mm) versus 8.9 mm (no Gd; CI: 4.0-13.9 mm, SD: 5.4 mm). The mean difference between pre- versus postcontrast was 0.7 mm (SD: 1.9 mm).
Numerous follow-up studies are now necessary to evaluate the software and its clinical utility, according to Dietzel. First, the size of the study collective must be increased to further validate the accuracy of the registration process itself. Second, it is essential to evaluate which clinical/pathological cofactors may be beneficial for accurate matching. For instance, small or early tumorous changes are likely to be less marked than advanced tumors showing massive desmoplastic reaction. The latter might be more difficult to co-register, but are easily diagnosed. The first group, including ductal carcinoma in situ -- i.e., preinvasive cancers -- could be easier to coregister. Such cases are probably more clinically relevant.
"Besides identifying clinically important subgroups, we are working on an improvement of the matching algorithm itself. With advancing informatics and finite element software, there is lots of space to further refine the matching accuracy," he commented.

 Dr. Matthias Dietzel (left) and his co-author Dr. Pascal A.T. Baltzer, both from the Institute of Diagnostic and Interventional Radiology at Friedrich-Schiller-University in Jena, Germany.
Dr. Matthias Dietzel (left) and his co-author Dr. Pascal A.T. Baltzer, both from the Institute of Diagnostic and Interventional Radiology at Friedrich-Schiller-University in Jena, Germany.