The more experience a radiologist has, the lower the risk of a false-positive result in breast cancer screening, according to a new study published in European Radiology. That may seem obvious, but to date the impact of radiologist experience on false-positive rates hasn't been studied much, or the results are contradictory.
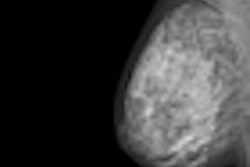
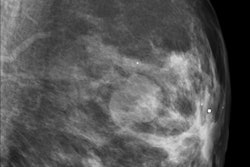
Biannual breast cancer screening, while beneficial, is not without its adverse effects, the most frequent being false-positive results. In this case, false positives were defined as the absence of histologically confirmed breast cancer after a positive screening mammogram and additional procedures. Researchers estimate the risk of a false-positive result varies from 20% to 50% for women participating in 10 screening rounds (i.e., women participating in biannual screening between the ages of 50 and 69, which the European Union recommends). Age, breast density, and a history of breast disease all influence false-positive results and cannot be changed. The number of views, type of reading, and radiologist's experience, however, can be modified.
Dr. Raquel Zubizarreta Alberdi and colleagues examined the factor of radiologists' experience in the context of a population-based program in Spain. In Spain and most other European countries, radiologists must interpret a minimum of 5,000 screening mammograms yearly to ensure quality. They divided false-positive results into two types: overall false-positive results, consisting of mammograms requiring additional assessment of any type to exclude malignancy, and false-positive results leading to at least one invasive procedure (Eur Radiol, 4 June 2011).
They found that out of more than 1 million single-read screening mammograms interpreted by 72 radiologists, the overall percentage of false-positive results was 5.85%. The percentage of false positives resulting in an invasive procedure was 0.38%. The risk of false positives overall and of false positives leading to an invasive procedure significantly decreased (p < 0.001) with greater reading volume in the previous year, wrote Alberdi, from the Galician Breast Cancer Screening Program and Public Health and Planning Directorate in Galicia, Spain.
Two variables were used to determine radiologists' experience at each reading: reading volume in the previous year as a measure of recent experience, and length of service in the breast cancer screening program as a measure of cumulative experience. Each radiologist's experience was recalculated for each mammogram interpreted since experience constantly changes.
An odds ratio (OR) of 0.77 and 0.78 was found for a reading volume of 500-1,999 mammograms. An OR 0.59 and 0.60 was found for a reading volume of more than 14,999 mammograms. The risk of both categories of false positives was also significantly reduced as radiologists' years of experience increased: OR 0.96 and OR 0.84, respectively, for one year of experience, and OR 0.72 and OR 0.73 for more than four years of experience.
The percentage of false-positive results decreased as women's age increased. This percentage also decreased in successive rounds compared with the first round. In addition, the percentage of false positives was greater with film-screen than with digital mammography.
"Given the recent introduction of digital mammography in screening programs, the tendency observed in this study should be investigated in future studies," the researchers wrote.
They also found the percentage of false-positive results overall decreased when two views were used rather than a single view. "However, the opposite effect was found for false-positive results leading to invasive procedures, a finding for which we have no explanation," the researchers wrote.
"The study results might be anticipated intuitively, but the study shows that the effect of the experience-related variables studied in the univariate analysis was similar to that observed in the multivariate analysis," Alberdi said in an interview with AuntMinnieEurope.com.
Alberdi and her team's results are in alignment with other studies with a slight difference. "Our results, although they also show a direct relationship between length of experience in the program and a reduction in false-positive risk, establish that this effect is of greater magnitude for reading volume in the previous year, recent experience thus having a greater effect than cumulative experience," they wrote.
The researchers are quick to point out their results are drawn from a retrospective cohort study analyzing mammography examinations performed in routine practice in screening programs, thus more closely reflecting the real risk of a false-positive result than other studies.
"This finding indicates that radiologist experience has a clear effect on false-positive results and is independent of the adjustment variables (women's age, screening type, number of views, mammography type, radiology unit, and period effect), allowing us to state the radiologist experience 'per se' affects the risk of a false-positive result," Alberdi said.