Computer-aided detection (CAD) can reduce the number of stereotactic breast biopsies of suspicious microcalcification clusters that are eventually shown to be benign, according to a German research team.
In a retrospective review of all stereotactic biopsies performed at their hospital in the previous year, researchers from Südharz-Krankenhaus Nordhausen found that CAD could potentially have avoided nearly half of these unnecessary biopsies.
"Despite double reading and [a] consensus conference, the sensitivity of stereotactically guided biopsy is still rather low," said Dr. Ansgar Malich, PhD. "CAD application in this specific subgroup of microcalcifications would yield an increased specificity and a slightly decreased sensitivity, and thus, an overall increased accuracy."
Malich presented the findings during a scientific session at ECR 2011 in Vienna.
The German mammography screening program features independent double reading of mammograms, with patients recalled in uncertain cases. Weekly case consensus conferences are held, and decisions to biopsy a suspicious microcalcification are usually made in consensus by the diagnostic and interventional radiologist, Malich said.
Reimbursement for stereotactic vacuum-assisted breast biopsy adds up to about 600 euros, but there is no reimbursement in Germany for breast MRI or any type of CAD application in a screening program.
Despite the double independent reading and the preinterventional consensus conference, however, the histopathologic outcome of stereotactic biopsies is not sufficiently high; sensitivity is about 50%, according to Malich.
As a result, the researchers sought to determine if CAD could play a useful role in reducing the unnecessary biopsy rate. They also wanted to evaluate if CAD would significantly influence sensitivity for BI-RADS B4 and B5a lesions and if it would be useful to introduce CAD reimbursement in a few selected cases.
They retrospectively reviewed 114 patients who had been screening-selected for biopsies of suspicious microcalcification clusters. No patients were excluded. All cases had proven extraction of the suspected microcalcification cluster and all interventions were successfully performed, he said. All biopsies provided a match of histopathologic and imaging findings, according to the postinterventional conference.
Of the 114 lesions that received biopsies, 59 were proved to be BI-RADS B2 (benign), while two were B3a. There were 14 B3b, four B4, 33 B5a, and two B5b lesions.
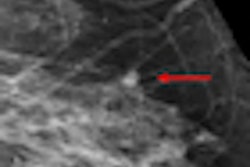
All cases were then analyzed utilizing the R2 CAD software (Hologic) with all three of the software's sensitivity settings. Two experienced radiologists then compared the CAD analysis with the imaging findings.
Each related CAD marker that hit the biopsied structures at least partially in one image was scored as positive. The marks that didn't were counted as false positives.
For biopsy-proven B3, B4, and B5 lesions, CAD yielded sensitivities of 84.9%, 88.7%, and 88.7% for its three different sensitivity settings. For B4 and B5 lesions only, CAD turned in sensitivities of 87.2%, 89.7%, and 89.7% for the three settings.
Perhaps most important, CAD correctly did not highlight B2 and B3a lesions in more than 40% of these cases; specificities were 47.5%, 47.5%, and 40% for the three CAD sensitivity settings.
Overall, CAD had negative predictive values of 78.4%, 78.1%, and 77.4% for its three settings, and positive predictive values of 58.4%, 57.3%, and 56.6%.
The false-positive rates for microcalcifications were 0.10, 0.18, and 0.20 per image for the three CAD sensitivity settings, and the false-positive rates for masses were 0.30, 0.41, and 0.50 per image. If CAD marks on histologically proven B2 lesions were included, those numbers increased slightly to 0.40, 0.48, and 0.55 for microcalcifications and 0.32, 0.42, and 0.53 for masses.
Malich noted that CAD's performance in this highly selected patient subgroup differs significantly from its application in a screening population.
"We have to take into account that the false-positive values of CAD, of course, are much higher than to be expected in a screening population," he said. "But on the other hand, all of the cases we included were judged to be suspicious enough to undergo biopsy, and so the specificity [of CAD] of up to 50% seems to be quite high because the radiologists and the consensus conference had a specificity of zero."
Some unsolved questions remain, however, Malich said.
"Is a slight decrease in sensitivity of approximately 10% acceptable when we are able to raise our specificity to up to 50%?" he said. "And how do we interpret [CAD results for] B3 lesions?"
Based on their results, Malich suggested that the CAD be applied with the highest sensitivity settings for microcalcification clusters being scored as BI-RADS 4. Those lesions with non-CAD-highlighted microcalcification clusters should be downstaged, he said.
Further scientific analysis is necessary to prove these findings, and cost-saving analysis should also be performed, Malich noted.