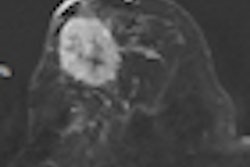
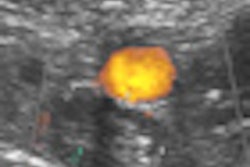
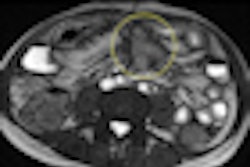
Screening mammography's sensitivity can be hindered after women have had conservative breast surgery or radiotherapy -- due to scars, changes in the breast's contours, skin thickening, and calcifications. But even benign surgery such as biopsy or breast reduction can cause permanent postoperative changes that decrease mammography's screening sensitivity, thus boosting the potential for higher recall rates, researchers from the Netherlands have found.
Although there are screening guidelines in Europe and the U.S. for interpreting mammograms after a woman has had surgery as breast cancer treatment, there are few guidelines for interpreting mammograms after a woman has had benign breast surgery.
Dr. Vivian van Breest Smallenburg, from Catharina Hospital in Eindhoven, sought to determine whether mammography's impaired sensitivity after benign breast surgery is due to postsurgical mammographic alterations or specific breast tissue characteristics, such as tissue density or fibrocystic changes. The team found that previous benign breast surgery does decrease mammography screening sensitivity due to postoperative mammographic changes (European Journal of Cancer, 18 April 2012, epub ahead of print).
"To our knowledge, this is the first analysis investigating the causes of lower sensitivity of screening mammography for cancer detection in a breast following ipsilateral benign breast surgery," van Breest Smallenburg and colleagues wrote. "[Our] study shows a lower sensitivity of screening mammography after previous benign breast surgery and we found that this lower sensitivity is most likely to be the result of postoperative mammographic changes rather than differences in breast density or the presence of specific tissue characteristics [such as density or fibrocystic changes]."
Surgical or tissue changes?
Her group included 351,009 screening examinations in 85,274 women that were taken between January 1997 and January 2009. The examinations of women with screen detected cancers or interval cancers, diagnosed after previous benign breast surgery, were reviewed by two screening radiologists who classified breast density and determined both the presence and degree of postsurgical changes and whether mammographic interpretation was hampered by tissue characteristics. Screening interval was approximately two years. The most frequent reasons for benign surgery were removal of palpable lesions such as fibroadenomas or cysts, mastitis treatment, and breast reduction, according to the group.
The study found that during the timeframe, 13.1% (46,155) of the total screens were initial screens, and 86.9% (304,854) were subsequent screens. Altogether, 1.3% (4,450 of the total number of screens) were referred for further diagnostic examination; of these, 1,772 had histologically proven breast cancer, yielding an overall cancer detection rate of five per 1,000 women screened and a true-positive referral rate of 39.8%, the team wrote. A total of 671 interval cancers were diagnosed at two-year follow-up, resulting in a screening sensitivity of 72.5% for breast cancer detection and an interval cancer rate of 1.9 per 1,000 screens.
One hundred and fifteen screen-detected cancers and 66 interval cancers (for a total of 181) were diagnosed in women who had had previous benign breast surgery. The Eindhoven group found that screening sensitivity was lower in women who had undergone prior benign breast surgery than those who had not: 63.5% as compared to 73.5%, respectively.
The researchers found that, after benign breast surgery, 49.6% of screen detected cancers and 53% of interval cancers had mammographic changes. Mammographic changes after surgery in the part of the breast where cancer was diagnosed were more distinct in interval cancers than in screen-detected cancers; women in this category also had an increased interval cancer risk.
Breast tissue characteristics did not prove to be strong influencing factors in the sensitivity of mammography screening after benign breast surgery, the team concluded: Hampered mammographic interpretation as a result of breast tissue characteristics was present in only three screen-detected cancers (two cases of fibrocystic changes and one case of multiple coarse calcifications) and one interval cancer (fibrocystic changes), according to van Breest Smallenburg.
The study's findings may have implications for future screening guidelines.
"At screening, utmost attention should be paid to mammographic breast segments showing changes in order to reduce the risk of interval cancer," she noted. "In order to prevent an adverse effect on screening sensitivity, excision of breast lesions with conclusive, benign pathology at percutaneous biopsy should only be considered if a woman persists on removal of the lesion."