For individuals who need a highly accurate colon screening exam but can't tolerate a full bowel prep, nonlaxative PET/CT colonography may be just what the doctor ordered, according to a new study from the U.K. published online this month in the Journal of Nuclear Medicine.
Researchers from University College London found that while PET/CT had about the same sensitivity as virtual colonoscopy, the combined modality had a sharply higher specificity and positive predictive value (PPV). This indicates that patients who have normal PET/CT colonography exams could be sent home safely without the need for further tests.
Purging and compliance
Virtual colonoscopy (also known as CT colonography or CTC) has proved its mettle for diagnosing colorectal neoplasia, and it's an attractive screening option for symptomatic older patients who are at increased risk of complications from colonoscopy, but who have a low cancer incidence of 10% or less, wrote Dr. Stuart Taylor and colleagues. But the bowel purging regimen required with the procedure can turn off many patients.
"There is evidence ... that arduous bowel purgation not only is detrimental to compliance, but also may cause serious adverse effects including significant electrolyte imbalance," the authors wrote. This has led to significant efforts in recent years to create an easier prep using stool and fluid tagging that enable reduction or elimination of laxative purgation (JNM, May 19, 2010).
As promising as the minimal-prep exams are, however, both sensitivity and specificity are generally lower than that of standard virtual colonoscopy with laxative-based purgation, even for large colonic lesions, Taylor and colleagues wrote. One alternative, PET/CT colonography, has been described previously, but its use has been limited to small studies examining its technical feasibility.
Therefore, the study aimed to "prospectively test the technical feasibility and patient acceptability of nonlaxative PET/CT colonography for the diagnosis of colorectal neoplasia in older patients at higher risk and to provide pilot data on diagnostic performance," they wrote.
The researchers recruited patients at high risk of colorectal neoplasia, including patients who had experienced a significant change in bowel habits, were undergoing polyp surveillance, had a family history of colorectal cancer, or had a positive fecal occult blood test. Excluded were pregnant patients, or those with a known diagnosis of inflammatory bowel disease, which can by itself increase F-18 FDG uptake.
Between April 2007 and April 2009, the researchers examined 56 patients (median age, 64 years; range, 46-83; 30 women, 26 men) using nonlaxative PET/CT colonography. Of these, 19 were examined because of fecal occult blood tests; 13 due to a change in bowel habits, 19 due to a family or personal history of colorectal cancer, and five because of rectal bleeding.
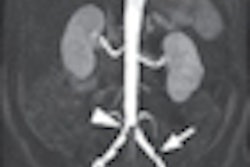
The day before the exam, patients followed a low-fiber diet and consumed a barium tagging agent (Tagitol V, Bracco Imaging, Milan, Italy). PET/CTC was performed following injection of 85 MBq of F-18 FDG (effective dose, 4.75 mSv) and 20 mg of hyoscine butylbromide (Buscopan, Boehringer Ingelheim, Ingelheim, Germany), as well as automated CO2 insufflation (ProtoCO2l, Bracco) of the colon.
Prone and supine CT data were acquired (1.25-mm collimation, 140 kVp, and 80-120 mA depending on body mass index) in conjunction with prone and supine PET acquisition using three bed positions to encompass the colon and an eight-minute acquisition per position, Taylor and his team wrote. Patients also underwent conventional colonoscopy, which served as the reference standard.
An experienced radiologist and a nuclear medicine physician examined each dataset and compared it to reference colonoscopy. Patients completed a 25-question survey discussing satisfaction, worry, and discomfort with the exam.
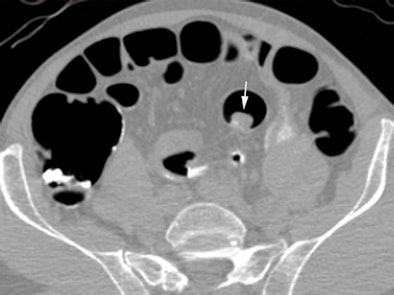 |
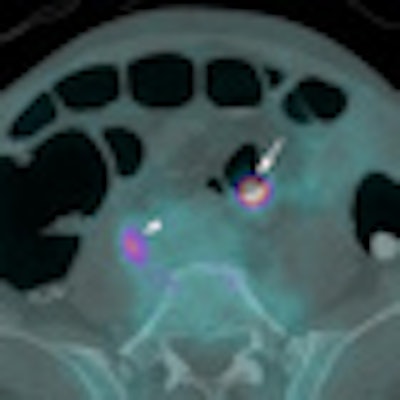
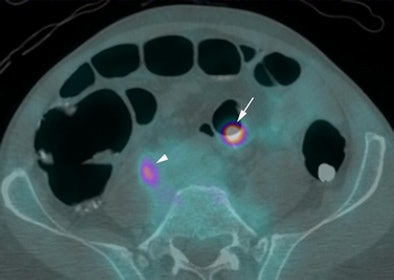
| Above, supine virtual colonoscopy image shows a 20-mm adenoma (arrow) in the sigmoid colon. Below, fused PET/CT in the same patient shows an area of intense F-18 FDG uptake corresponding to the 20-mm adenoma. A small amount of misregistration is present. Arrowhead points to ureteric activity. All images courtesy of Dr. Stuart Taylor. |
 |
The results showed good distention in 298 of 334 segments (89%, 95% confidence interval [CI]: 85%-92%). Patients experienced more physical discomfort during colonoscopy (median, 4; interquartile range [IQR], 2-7) than during the PET/CT colonography exam (median, 5; IQR, 3-7; p = 0.03).
Patients also more often expressed willingness to undergo PET/CT colonography again (36 of 43, or 84%; 95% CI: 73%-95%), compared to 31 of 43 (72%, 95% CI: 59%-86%, p = 0.001) who expressed a preference for conventional colonoscopy.
As for lesions, 21 patients had 54 polyps according to the colonoscopy results, 10 of whom had at least one polyp larger than 6 mm and eight of whom had at least one polyp larger than 10 mm.
Of the 14 polyps that were 6 mm or larger in diameter, 12 (86%, 95% CI: 67%-100%) were avid for F-18 FDG, including all of the lesions 10 mm or larger (mean standardized uptake value [SUV], 10.1), Taylor and his team wrote. Moreover, the group found no significant difference in mean SUV for adenomas with (mean, 12.7) and without (mean, 7.4) high-grade dysplasia (p = 0.10).
A single 6-mm polyp missed on CTC was not F-18 FDG-avid, nor was there uptake in any polyp 5 mm or smaller.
Similar sensitivity, higher specificity
CTC's sensitivity for polyps 6 mm or larger of 92.9% (95% CI: 79.4%-100%) did not improve with the addition of PET. However, the combined exam did improve the per-patient positive predictive value for a polyp 10 mm or larger from 73% (95% CI: 39%-92%)to 100% (95% CI: 60%-100%).
Extracolonic findings -- all detected by the CT component of the exam -- were reported in 12 patients, not including those with simple liver and renal cysts. The findings included large uterine fibroids (two patients), gallstones (two patients), gastric carcinoma, a benign presacral mass (little F-18 FDG avidity) renal obstruction (two patients), an adrenal mass (non-FDG-avid and benign on workup), an enlarged prostate, and pancreatic atrophy (two patients).
"In this feasibility study, simultaneous PET acquisition during nonlaxative CT colonography is technically feasible, is well tolerated, and potentially improves specificity," Taylor and colleagues wrote.
"Reassuringly, PET/CT colonography detected all polyps 10 mm or larger, and all were F-18 FDG avid," they wrote. "However, only half those that were 6-9 mm and no polyps that were 5 mm or smaller were F-18 FDG avid."
Patients preferred the minimal PET/CT colonography bowel preparation "and reported significantly more physical discomfort during colonoscopy, despite sedation and the long examination time of the PET/CT colonography itself (55 min)," the authors wrote. "Both factors likely explain the overall patient preference for PET/CT colonography over colonoscopy. Also, although our regimen was laxative-free, patients did still need to modify their diet." A study with no dietary modifications is worthy of pursuit, they added.
The utility of PET for detecting recurrent colorectal malignancy is established; however, its role in primary diagnosis is uncertain, the authors wrote, citing a recent study of 110 asymptomatic individuals. In that study, 61% of 23 adenomas 10 mm or larger were visible restrospectively as F-18 FDG-avid foci, although lesions 9 mm or smaller were apparently undetectable, they wrote. Another study showed a similar lack of avidity for small lesions. Even large polyps that are clearlyvisible at CTC sometimes show no F-18 FDG uptake, suggesting that factors other than size influence F-18 FDG avidity.
"We found the PPV of PET/CT colonography reassuringly high, albeit in our small pilot study of diagnostic performance," they wrote. "A normal PET/CT colonography result would be highly reassuring, thus obviating further investigations. Conversely, a positive result would be sufficiently concerning to justify more invasive tests."
Simultaneous PET acquisition during nonlaxative virtual colonoscopy is technically feasible and well tolerated by patients, the group concluded. This study demonstrates that it can potentially improve specificity, confidence, and positive predictive value, although not sensitivity.
"Use of this specialized technology will likely be reserved for patients intolerant of full bowel laxation in whom a sensitive and highly specific test is required to exclude significant colonic pathology," Taylor and colleagues concluded.
By Eric Barnes
AuntMinnie.com staff writer
May 27, 2010
Related Reading
Medicare coverage spurs 41% growth in colorectal cancer PET use, January 26, 2010
FDG-PET/CT trumps CT in detecting anal carcinoma, November 25, 2009
FDG-PET detects recurrence of colorectal cancer early, April 3, 2008
Combined PET and CT detects colorectal cancer recurrence, metastasis, October 25, 2007
PET/CT improves diagnostic accuracy of unexpected malignancies, June 30, 2005
Copyright © 2010 AuntMinnie.com