Italian researchers have concluded that MRI shows high sensitivity for the detection of osteomyelitis in a diabetic foot, but lower specificity related to Charcot neuropathic osteoarthropathy.
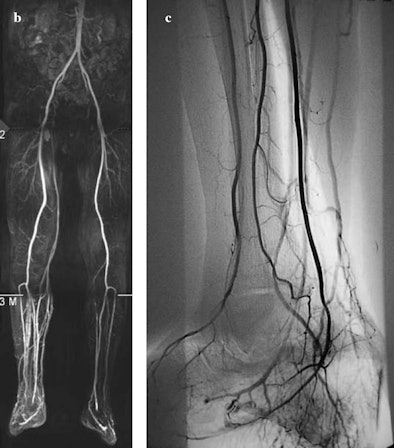
In addition, inflammatory hyperaemia caused by the ulcer can deteriorate the diagnostic quality of 40% to 50% of MR angiography studies in the infrapopliteal region. If and when that occurs, the researchers recommend selective arteriography.
The study comes from Carlo Poma Hospital in Mantua, Italy, and was published online on October 25 by La Radiologia Medica.
Foot ulcers are usually the earliest warning sign in diabetic patients and 15% of cases develop into osteomyelitis. Early recognition of osteomyelitis guides medical and surgical treatment, which are usually implemented in an inpatient hospital setting.
The clinical diagnosis of the infected foot is problematic in diabetic patients because as many as two-thirds of patients may not present with the classic symptoms of deep infection, due primarily to immunodeficiency and diabetes mellitus.
The study noted that while bone probing through skin ulceration offers positive predictive value of 89% in the diagnosis of foot osteomyelitis, its low sensitivity of 66% does not exclude bone infections. As a result, diabetic patients with suspected foot osteomyelitis require musculoskeletal imaging for diagnosis and evaluation of the extension of the infection to plan surgery and avoid recurrences.
Patient demographics
The Italian study, co-authored by Dr. Roberto Caudana, retrospectively reviewed 16 diabetic patients (11 men and five women) with a mean age of 58 years between January 2006 and September 2007. All musculoskeletal MRI examinations were conducted with a 1.5-tesla MRI unit (Magnetom Avanto, Siemens Healthcare, Erlangen, Germany) and an extremity coil.
In 10 cases, patients had a unilateral infected ulcer affecting the forefoot; two cases involved the midfoot, and four cases involved the hindfoot. All patients underwent radiographic foot scans, which proved positive for osteomyelitis in seven of 16 patients.
The clinical indication for MRI in seven of 16 patients was to assess the extent of osteomyelitis. In the other nine patients, MRI confirmed or excluded the suspicion of osteomyelitis, even when there were no radiographic signs of bone infection. In three of nine cases, there was a prevalence of bone rarefaction, fractures, fragmentation, dislocation, or reparative osteoblastic response.
Based on the suspicion of peripheral arteriopathy, 12 of 16 patients with an infected diabetic foot also underwent MR angiography with a contrast agent three days to six weeks after an MRI scan of the foot, using the same scanner.
Study results
Researchers determined that in 13 of 16 patients with infected diabetic foot ulcers, the final diagnosis was osteomyelitis; in three of 16 cases, the diagnosis was cellulitis.
In the osteomyelitis cases, there were 13 true positives, one false positive, and two true negatives. In the one false-positive case, CT-guided bone biopsy allowed exclusion of osteomyelitis and demonstrated only reactive bone marrow oedema.
MRI correctly ruled out osteomyelitis in two patients with infected ulcer and cellulitis true negatives, in which conventional radiology identified alterations due to neuropathic osteoarthropathy.
Overall, the MRI scans of the foot correctly identified or excluded osteomyelitis in 15 of 16 patients, with a high accuracy and sensitivity, even in the three cases of radiographic evidence of neuropathic osteoarthropathy.
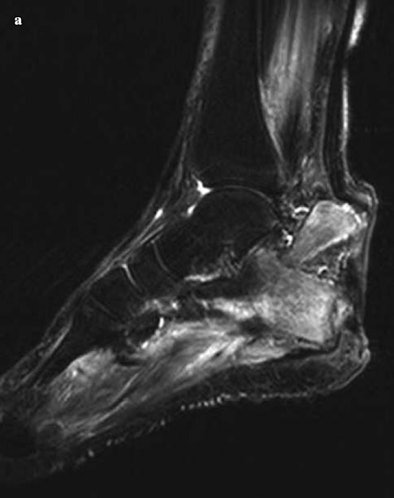 |
| The images show osteomyelitis of the calcaneus due to infected neuropathic ulcer of the heel. In (a), the sagittal short-tau inversion-recovery sequence image shows a pathological fracture of the calcaneus and dislocation of the proximal fragment due to retraction of the Achilles tendon. In (b), MR angiography of the right lower limb is hindered by venous contamination in the distal third, whereas the left infrapopliteal arteries are clearly visible up to the plantar arch. In (c), selective arteriography of the right lower limb shows normal infrapopliteal arteries and early venous filling due to inflammatory hyperaemia. Images courtesy of La Radiologia Medica and Carlo Poma Hospital, Mantua, Italy. |
 |
Assessing osteomyelitis
The study also noted that MRI "also proved useful for assessing the extent of osteomyelitis for surgical planning purposes (four minor and one major amputation), for identifying soft-tissue abscesses requiring drainage (three cases) as well as other infectious complications including septic arthritis (four cases), pathological fracture (one case), and septic tenosynovitis (one case)."
"The combination of primary and secondary MRI signs and their topographic concordance are essential for improving the specificity of the examination," the researchers wrote.
In doubtful cases, they added, image-guided bone biopsy remains the only technique capable of identifying false-positive results on MRI, due to neuropathic osteoarthropathy. Bolus-chase MR angiography of the lower limbs also is the preferred vascular study in diabetic patients for planning peripheral revascularization.
By Wayne Forrest
AuntMinnie.com staff writer
November 10, 2008
Related Reading
FDG-PET may supplement MRI for acute osteomyelitis, August 25, 2008
SNM's Images of the Year show molecular imaging's head-to-toe prowess, June 16, 2008
CMS declines PET coverage for infection, inflammation, March 20, 2008
SPECT/CT offers better bone scan views to enhance treatment, September 21, 2007
SPECT/CT offers on-target diagnosis in noncancerous bone disease, March 23, 2007
Copyright © 2007 AuntMinnie.com