Calcaneal fractures are subtle injuries that require an urgent diagnosis because they can have long-term disabling consequences if not treated early, Spanish musculoskeletal (MSK) experts stated in a top award-winning e-poster at last week's European Congress of Radiology (ECR).
"Its main manifestation [heel pain] can go unnoticed in the context of a major multiple trauma in which other fundamental structures of loading axis [spine] may be affected. Correct diagnosis and characterization of the injury in an early stage is crucial to improve therapeutic options and prognosis of this disease," noted lead author Dr. Jose Carlos Rayón-Aledo, from the Servicio de Radiodiagnóstico in Madrid, who received a Magna Cum Laude award at ECR 2012 for his research.
Digital x-ray remains a key tool of investigation. A high level of clinical suspicion and a detailed imaging study in all three planes of space is desirable for proper treatment planning and to estimate the prognosis, according to Rayón-Aledo. The multiplicity of fracture lines and the different levels at which they occur explain how an injury can easily go unnoticed. The minimum images required are lateral and axial scans of the foot, plus bilateral images, but it is not uncommon to need other complementary projections.
A calcaneal fracture is associated with axial load mechanisms, usually car accidents or falls from great heights. Around 60% are tarsal fractures, and the typical patient is a man between 30 and 60 years of age. It is important to consider the possibility of bone fractures in segments that absorbed the energy of the impact, such as the contralateral calcaneus, tibia and tibial plateau, femur and its proximal epiphysis, spinal cord, and cervical spine and atlanto-occipital articulation.
The signs and symptoms include severe heel pain on percussion of the heel, severe pain when the patient attempts inversion or eversion of the foot, and increased volume of the entire body of heel and ankle. A plantar bruise appears rarely.
"In any patient who has fallen standing up, with the support of one or both heels, regardless of the height of the fall, with slight pain on percussion of the heel, with slight difficulty walking or when stepping on the toes, a calcaneal fracture should be considered," explained Rayón-Aledo, adding that the possibility of injury of the neurovascular axis during trauma or fragment reduction surgery is a key factor in surgical decision-making.
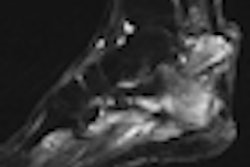
Digital x-ray doesn't always lead to a definitive diagnosis, and CT may be necessary to differentiate fractures suitable for surgical repair from inoperable ones, to define different fracture lines and planes in which they spread, to describe the exact location of the fracture line in the posterior articular facet, and to locate precisely the fracture and its relation to the lateral malleolus and the peroneal tendon.
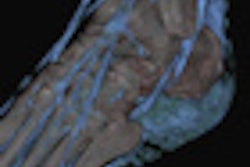
"Multislice CT allows us to obtain detailed images of the calcaneus setting, the subtalar joint, and the main visual axis, so we can specify intra-articular involvement and classify the fracture [Salter-Harris], taking into account the different prognosis and treatment considerations that this classification entails," the authors noted. "We may reformat the images using the posterior facet of the talus calcaneus joint as the main axis. A correct planification is critical to be able to obtain critical information."
Intra-articular fractures can be defined by disruption of the posterior facet. Some signs that may help indicate their presence are soft-tissue damage, loss of height, and widening. Intra-articular fractures should be classified for an optimal evaluation, and the best correlation to management and prognosis is found in the Sanders classification system, based on the location of the fracture line in the posterior facet of the subtalar joint, they stated. Calcaneal fractures do not affect the subtalar joint in about 25% to 30% of cases.
Extra-articular fractures have a good prognosis, are simple to treat, and, in general, have no functional sequelae. They do not undertake support joint surfaces and are most frequently associated with soft-tissue edema. The fracture lines are short, and the bone fragments are usually embedded or the degree of separation is usually very small. If reduction becomes necessary, it is achieved with manual compression measures, the authors wrote.
The definitive treatment can be conservative or surgical and depends on the type of fracture (intra- or extra-articular), displacement of the fragments, and the patient's age, level of work activity, and general condition. Conservative treatment is recommended in extra-articular fractures or intraclosed without displacement or with a small displacement (1-2 mm), or in patients unsuitable for surgery. It involves eight weeks without load-bearing activity, followed by some walking with partial load-bearing movement. In open fractures and closed fractures with a displacement greater than 2 mm, the surgical options are arthrodesis, fixation of percutaneous cannulated screws and needles, or open reduction and osteosynthesis with plaques.
Complications are often directly related to a delay in diagnosis and treatment. They may include tendon injuries or entrapment of adjacent structures, infection (20% of cases), and loss of supination, pain, lameness, and enlargement of the hindfoot, making it to difficult to wear shoes.
"Classic findings in simple radiology [abnormalities in Gissane and Böhler angles and Nelaton triangle] seem overwhelmed by the information provided by multislice CT with coronal and sagittal reconstructions," the authors concluded. "However, its knowledge is very useful to understand the different mechanisms of injury and to be able to diagnose this pathology in a daily practice, possibly away from 3D technologies."