MRI is the best modality to evaluate musculoskeletal (MSK) infections because it confirms the clinical diagnosis, delineates disease extent, and reveals complications, particularly in the foot, Portuguese researchers said at the recent European Society of MR in Medicine and Biology (ESMRMB) congress in Lisbon.
"Contrast administration appears most useful for characterization of soft-tissue abnormalities including abscess, phlegmon, sinus, and fistulous tracts. It may also help in cases of chronic osteomyelitis," noted Dr. P. Diana Afonso, from the department of radiology at Hospital da Luz -- Espirito Santo Saude in Lisbon. "The presence of Charcot arthropathy (or neuropathic arthropathy, which affects some diabetic patients with peripheral neuropathy) remains a confounder in this population group."
MRI has developed an essential role in assessing MSK pedal infections, and makes it possible to verify the presence of an infection and its extent. Combining unenhanced and static-enhanced sequences often is used in clinical practice, but this area still is a focus of debate amongst MSK specialists.
"Many radiologists avoid contrast administration due to increased expense, longer magnet time, and safety issues -- principally nephrogenic systemic fibrosis. Others add contrast presuming a more definitive diagnosis will be obtained, resulting in better management and a final cost saving," she explained.
MSK infections are common and seem to be increasing. In the U.S., nearly 2 million patients are diagnosed and treated annually for these infections. They comprise a spectrum of disorders determined by which tissues are involved: soft tissues, bones, and joints. MSK infections are particularly challenging in the foot, where multiple structures are tightly packed together, according to Afonso.
Pedal infections are increasingly common, particularly in patients with diabetes and those who are immunocompromized. They can be limb- or life-threatening, and the speed and accuracy of a diagnosis has an impact on immediate treatment and potential complications.
To draw up her analysis, Afonso studied 80 MRI examinations retrospectively. The patients presented with the clinical indication of infection of the foot/ankle and/or toes. All were imaged with T1-weighted spin echo, T2-weighted fast spin echo, or short tau inversion recovery (STIR) and postcontrast T1-weighted spin echo, performed at either 1.5 tesla or 3.0 tesla. Patients' electronic clinical records were reviewed, and imaging findings were correlated with clinical history and final diagnosis.
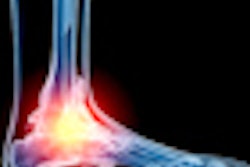
On unenhanced MRI, osteomyelitis was primarily defined as focally decreased signal intensity on T1-weighted images and focally increased signal intensity of bone marrow on fluid-sensitive sequences, with marrow enhancement after contrast administration. Secondary signs for osteomyelitis were defined as cortical destruction, intraosseous or subperiosteal rim-enhancing fluid collections, sequestrum, sinus tract, and surrounding cellulitis. MR criteria of septic arthritis include joint effusion with synovial thickening that enhances on postcontrast imaging.
"Primary signs of osteomyelitis include abnormal marrow signal on all pulse sequences. Secondary signs increase specificity and include bone destruction and adjacent soft-tissue abnormalities," she concluded.