Even in patients with well-controlled heart rates, dual-source coronary CT angiography (CTA) delivers significantly higher specificity and accuracy per coronary segment compared to 64-detector-row CTA, concludes a new study from Switzerland.
Nevertheless, the practical differences appeared to be small inasmuch as per-patient accuracy was equivalent, and image quality was excellent for both types of scanners, according to a Radiology study published online ahead of print (July 8, 2009).
"Owing to scanner-specific settings, including the heart rate-adapted pitch, dual-source CT coronary angiography has been shown to be associated with similar or even lower radiation dose levels as compared with 64-section CT coronary angiography, particularly at higher heart rates," wrote Dr. Stephan Baumüller and colleagues from University Hospital Zurich in Switzerland.
"Interestingly, although many studies have evaluated the feasibility, accuracy, and radiation dose of dual-source CT coronary angiography at higher heart rates, to our knowledge, no study so far has investigated whether the higher temporal resolution of dual-source CT would also have a beneficial effect on the accuracy at heart rates of 65 beats per minute or less," they added.
Two cohorts
To compare the two scanners at these heart rates, the study included 200 patients scanned with either dual-source coronary CTA or 64-section coronary CTA.
The first cohort of 100 consecutive patients (28 women, 72 men; age range, 30-83 years; mean age, 62 ± 11 years) was scanned using a 64-detector-row CT scanner (Somatom Sensation, Siemens Healthcare, Erlangen, Germany). The second cohort (30 women, 70 men; age range, 27-86 years; mean age, 61 ± 11 years) was examined with a dual-source CT scanner (Somatom Definition, Siemens Healthcare).
Two independent observers blinded to the angiography results independently assessed the image quality of all coronary segments on a four-point scale (1 = excellent) and searched for significant (> 50%) stenoses in each segment. Catheter angiography served as the reference standard.
All patients had typical or atypical chest pain and low to intermediate risk of cardiovascular disease, the researchers reported. Exclusion criteria included nephropathy, hypersensitivity to contrast media, nonsinus rhythm, and previous coronary intervention or stent implantation. All 200 patients underwent catheter angiography within four weeks of coronary CT angiography (median, 10 days).
The patients were scanned using retrospective electrocardiogram (ECG)-gated coronary CTA on one of the two scanners from the tracheal bifurcation to the diaphragm, with ECG-controlled tube current modulation for radiation reduction. All scans used 0.6-mm thick sections, 120 kV, and 600-850 mAs (64-detector) or 350 mAs per tube (dual-source). The center of the pulsing window was 70% of the RR interval for 64-detector scanning and adjusted to the patient's heart rate for dual-source imaging, the authors wrote.
When not contraindicated, 100 mg of IV metoprolol was administered an hour before CT when the heart rate exceeded 65 beats per minute. Patients also received an oral dose of 2.5 mg isosorbide dinitrate as a beta-blocker three minutes before scanning.
After an unenhanced scan for Agatston scoring, patients received 70-100 mL (adjusted to body weight and scan time) iodinated contrast followed by a 40-mL saline flush using a dual-head power injector at 5-6 mL/sec.
Images were reconstructed into 3-mm-thick nonoverlapping sections at 70% of the RR interval, using additional reconstructions when motion artifact was present.
Among 1,405 dual-source and 1,387 64-detector-row images evaluated, no significant differences were found in image noise levels between 64-detector-row (27 HU ± 6; range, 18-40 HU) and dual-source (27 HU ± 5; range, 18-35 HU; p = 0.97) CT scanners.
Interobserver agreement was significant (k = 0.71) for image quality between readers, and no significant difference was found in the number of nonassessable coronary segments between dual-source (1.0%, 14 of 1,405) and 64-section coronary CT angiography (1.8%, 25 of 1,387; p = 0.08).
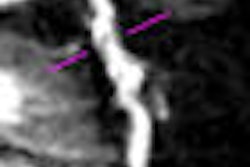
Motion artifacts with single source
Yet motion artifacts were far more common with the 64-detector-row scanner (21/25) than the dual-source system (5/14, p = 0.004), the report concluded, and segment-based accuracy and specificity were significantly higher for dual-source versus 64-section coronary CTA.
Per-patient and per-vessel accuracy did not differ significantly between the scanners, and no significant differences (p = 0.13) were found in the effective radiation doses (dual-source: 10.9 mSv ± 1.1; 64-detector: 10.4 mSv ± 1.7).
"Poor image quality was most often present in distal coronary segments and side branches" comprising 11 of 14 segments in dual-source CT and 14 of 25 segments in 64-section CT. For middle coronary segments, poor image quality was present in three of 14 segments in dual-source and 11 of 25 in 64-detector CT images, and there was no poor image quality in proximal segments, the group wrote.
"The accuracy (p = 0.01) and specificity (p = 0.04) were significantly higher with dual-source CT coronary angiography when compared with 64-section CT coronary angiography in the segment-based analysis," they wrote. "There were no significant differences in the vessel- and patient-based analyses regarding specificity (p = 0.06 and 0.08, respectively)."
The radiation hit was similar, lacking significant differences between scanners in effective dose (p = 0.13), CT volume dose index (p = 0.96), scan length (p = 0.15), or dose-length product (p = 0.13).
"In patients with heart rates of 65 beats per minute or less, the higher temporal resolution of dual-source CT coronary angiography results in improved accuracy and specificity for the diagnosis of significant stenoses on a per-segment level at a similar radiation dose, but provides a comparable diagnostic accuracy on a patient-based level as does 64-section coronary angiography," Baumüller and his team wrote.
The higher temporal resolution of dual-source CT provides a further increase in specificity and accuracy for diagnosing significant stenoses in a per-segment analysis.
However, "the differences in diagnostic accuracy parameters between both CT systems were not significant in the vessel- and patient-based analyses. In a clinical setting, the patient-based analysis is the most important result because only this one indicates whether a patient needs further invasive workup," they explained.
As for limitations, although vessel- and patient-based analyses showed no differences in diagnostic accuracy, with only 200 patients "the study seems to be underpowered to draw firm conclusions" in this regard, the authors wrote. They added that the study used different cohorts for the different scanners, and did not take advantage of newer prospective gating techniques that could have lowered the radiation dose further.
Baumüller and colleagues concluded that in patients with heart rates of 65 beats per minute or less, the two scanner types have comparable diagnostic accuracy on a patient-based analysis. Radiation dose using retrospective gating is also similar.
However, dual-source coronary CTA "has a significantly higher specificity and accuracy at segment-based analysis than does 64-section CT for the diagnosis of coronary artery stenoses," they added. Dual-source also boasts fewer nondiagnostic segments due to motion artifacts compared with 64-section CT.
By Eric Barnes
AuntMinnie.com staff writer
August 7, 2009
Related Reading
Dual-source CTA turns in mixed results for coronary stenoses, July 30, 2009
Prospectively gated coronary CTA nearly equals normal-dose scans, July 17, 2009
Triple-rule-out CT scans benefit from prospective gating, May 28, 2009
Wide-area CT detectors boost some clinical applications, May 20, 2009
Stress MPI with Tc-99m SPECT identifies high-risk obese patients, September 1, 2006
Copyright © 2009 AuntMinnie.com