Advances in CT and MRI mean it's feasible now to identify subtle cardiac pathologies responsible for stroke that used to remain unnoticed, and this is putting greater emphasis on the know-how of imaging professionals, according to Spanish researchers who received a prestigious magna cum laude award at ECR 2017.
"Radiologists play a pivotal role in stroke diagnosis and management," noted Dr. Flavio Zuccarino and colleagues from the thoracic radiology section in the department of radiology at Hospital del Mar in Barcelona, Spain. "Radiologists should be able to recognize these findings in order to perform an accurate diagnosis, which is of great value for patient management."
Brain infarction is the second most common cause of mortality worldwide and the third most common cause of disability, and while the overall rate of stroke-related mortality is decreasing, the absolute number of people with stroke and the global burden of stroke-related disability are high and increasing, they explained in the prize-winning e-poster presented at the Vienna congress.
The authors highlighted the following three main subtypes of brain ischemia:
- Intravascular thrombosis, which refers to obstruction of an artery due to the formation of a thrombus generally after arterial wall disease, such as arteriosclerosis, dissection, or fibromuscular dysplasia.
- Embolism, which refers to occlusion of cerebral vessels with debris of extracerebral origin, most commonly cardiac. An embolus may consist of platelet aggregates, thrombus, platelet-thrombi, cholesterol, calcium, bacteria, etc. Further events may occur if the embolic source is not identified.
- Systemic hypoperfusion, which refers to a diminished vascular supply due to several causes, most related to cardiac dysfunction (myocardial ischemia, cardiac arrest, arrhythmias). It may affect the brain and also other organs.
Cardiogenic strokes are characterized by affecting proximal arteries with larger infarct areas, greater recurrence chance, and higher disability and mortality rates, they continued. The potential causes are shown in the table.
| Potential causes of cardiogenic stroke | ||
| Causes | High risk | Low risk or undetermined |
| Atrium (> left) |
|
|
| Ventricle (> left) |
|
|
| Valves |
|
|
"The underlying mechanism of cardioembolic stroke is obstruction of cerebral vessels with embolic debris of a cardiac origin, commonly from the left chambers," the authors wrote. "However, abnormal intracardiac communication between the right and left circulation together with a pressure gradient that promotes a right-to-left shunt, may lead to unnatural passage from the venous to the arterial circulation; this is known as a paradoxical embolism."
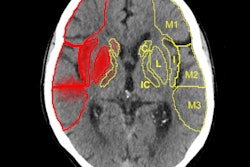
Emboli from the heart are distributed evenly throughout the body, yet more than 80% of symptomatic emboli affect the brain, they pointed out. The vascular territory affected is equivalent to the distribution of cerebral blood flow, and as much as 80% involve the anterior circulation (i.e., carotid artery region) and about 20% have a vertebrobasilar distribution.
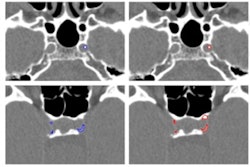
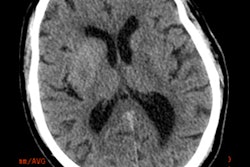
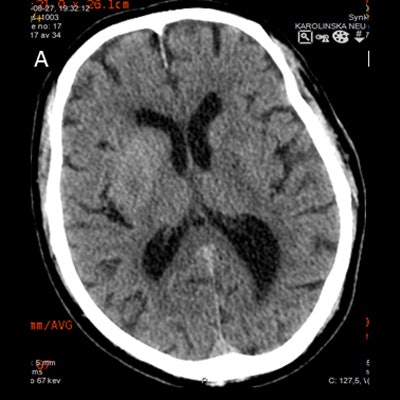
In brain CT and MRI studies, embolic infarctions appear as extensive or multiple lesions, simultaneously or sequentially affecting different arterial territories, corresponding to different emboli. Hemorrhagic transformation usually occurs in established ischemic lesions.
"Cardioembolic stroke is largely preventable with an optimal primary prevention," according to Zuccarino and colleagues. "When this is not achieved and stroke occurs, diagnosis of the potential cardiac source is fundamental to avoid further events."
Usually echocardiography is the initial cardiac imaging technique of choice because it is easily accessible, has a relatively low cost, and does not involve radiation exposure. Both transthoracic echocardiography and transesophageal echocardiography can be used. However, echocardiography has some limitations: It is operator-dependent, and some potential cardiac findings responsible for stroke may remain unnoticed.
In most patients with stroke of undetermined etiology or infarction with a suspected cardiac origin, no further cardiac evaluation is performed, they added.
"Revision of both thoracic CT and cardiac MRI studies (whether prior or coincident with the ischemic episode) can provide much information regarding a cardiac or large artery origin of stroke," the authors stated. "In recent years, cardiac CT is increasingly being used as a complementary imaging technique for cardiac assessment after echocardiography."
Some experts recommend early cardiac and extracranial vascular CT angiography, in addition to brain CT angiography, during the evaluation of patients with acute ischemic stroke. They advocate that an earlier risk factor management may reduce recurrence and improve outcome, while adding only few minutes to the protocol and making radiation dose increase feasible with adjusted protocols, they concluded.
To view the authors' extensive range of clinical cases presented at ECR 2017, click here.