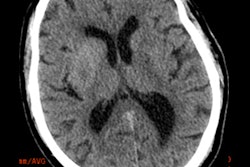
Advanced software can now be used to evaluate CT scans of stroke patients, assessing the severity of the stroke and helping to identify patients who will not benefit from thrombectomy, attendees learned at the 98th German Radiology Congress (Deutscher Röntgenkongress, RöKo 2017) in Leipzig.
Furthermore, computers can even establish the likely effect of therapy more objectively than experts who evaluate the images manually, according to Dr. Christian Herweh, a neuroradiologist at Heidelberg University Hospital and a speaker on the opening day of the four-day conference.
 Dr. Christian Herweh from Heidelberg. All images courtesy of the German Radiological Society.
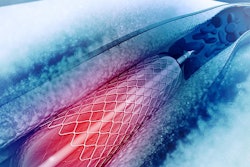
Dr. Christian Herweh from Heidelberg. All images courtesy of the German Radiological Society.The treatment of patients with ischemic stroke has changed dramatically in recent years. In the past, the standard therapy was intravenous lysis to dissolve blood clots in the brain. Today, thrombectomy offers a minimally invasive endovascular therapy shown in major studies to have clear benefits compared with lysis alone.
"As a result of these studies, thrombectomy is now being used for large numbers of patients," he said in advance of the congress. "But it's not always clear that every patient is actually benefiting from it."
This is a problem because thrombectomy is carried out mainly at larger centers to which patients must often be transported, and there is no point in exposing them to this unnecessary stress if they will not benefit from the intervention.
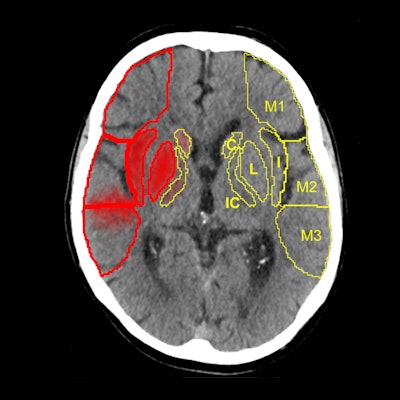
In large clinical studies, thrombectomy has been used mainly in patients whose CTs show a lower degree of severity, normally assessed using the Alberta Stroke Program Early CT Score (ASPECTS). In most of the successful studies, including ESCAPE, SWIFT PRIME, and REVASCAT, the ASPECTS must be no worse than six or seven points out of 10.
ASPECTS scoring is standard in patients who undergo CT for a recent stroke. "Doing the scores manually requires a high degree of experience, and is prone to error," Herweh said, adding that this problem can be solved by using software to calculate the scores. "It's more objective, and may be better than radiologists at evaluating patients' prognoses."

Computers versus experts
The Brainomix eASPECTS software, which has been around for some time now, is increasingly proving its value in clinical studies.
An initial validation study of 34 patients by the Heidelberg group showed that software evaluation of CT images was better than assessments by radiologists with limited training, and performed to the same level as experts. Furthermore, a U.K. study of 132 patients showed the software was at least equal to neuroradiologists, he explained.
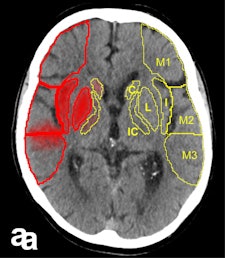
It works from a technical viewpoint, but the key clinical question is whether this method is better than, or as good as, experts at predicting which patients have a poor prognosis. Therefore, Herweh and his colleagues carried out a third study of 212 recent stroke patients, using three experts and the software to calculate the ASPECTS retrospectively. The result was then correlated with the patients' actual clinical progress.
"What we've shown is that the software reliably predicts a poor prognosis following thrombectomy," he stated.

A low eASPECTS has a statistically significant correlation to such a prognosis. Among experts, however, this correlation was statistically significant in only one out of three cases. In other words, software-based scoring could be more objective and clinically conclusive than manual scoring by experts.
"Of course, the software will never make treatment decisions on its own," Herweh concluded. "But it can provide valuable guidance in patients with borderline ASPECTS due to clear and early CT indications, which make therapy decisions more difficult."
Editor's note: This is an edited version of a translation of an article published in German online by the German Radiological Society (DRG, Deutsche Röntgengesellschaft). Translation by Syntacta Translation & Interpreting. To read the original article, click here.