The diagnosis of osteoporosis needs to improve significantly, according to a recent Australian study being highlighted in a press release issued on 9 September by Monash University in Melbourne, Australia.
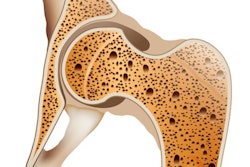
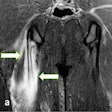
Osteoporosis affects one in three women and one in five men over the age of 50 and is responsible for more than 9 million bone fractures per year in women globally. The disease can be caught with an imaging tool called dual x-ray absorptiometry (DXA), which measures bone mineral density.
However, recent analyses suggest as many as 80% of scan reports contain errors, according to endocrinologist Dr. Amanda Vincent and Dr. Alicia Jones.
The International Society for Clinical Densitometry (ISCD) publishes criteria on the appropriate use of DXA in clinical settings. In this study, the researchers aimed to determine whether DXA reports for patients receiving care at a large academic teaching hospital in Melbourne are adhering to required ISCD reporting standards.
Writing in the Journal of Clinical Densitometry, the researchers manually compared 459 DXA reports with ISCD guidelines. The reports were from patients aged 18 years and over who received care at specialist outpatient clinics between January 1, 2018, and December 31, 2019.
The researchers found ISCD criteria with the lowest adherence scores regarded recommendations and timing of future DXA scans (included in just 1.1% of reports) and recommendations for investigations for secondary causes of osteoporosis (included in 1.2% of reports).
The fact that doctors have the technology for accurate diagnosis but are generally failing to apply best practice when using it is potentially a huge missed opportunity, the authors concluded.