A new method may help improve delineation between malignant and benign breast lesions on breast MR images, according to researchers from the University of Groningen in the Netherlands. The group won a prestigious magna cum laude award at ECR 2017 in Vienna for its work.
In their proof-of-principle study, the researchers compared the reproducibility and diagnostic use on breast MRI of three alternative methods comparing the apparent diffusion coefficient (ADC) values in regions of interest (ROIs) standardized by fixing both size and shape to cover the whole lesion. The team, led by Dr. Mirjam Wielema from the university's radiology department, found fixed size and shape ROIs are comparable with whole-lesion ROIs.
"The ADC values derived from fixed size and shape ROIs covering the geometric center of breast lesions or subregions of minimal ADC are equally reproducible as whole-lesion ROIs," they noted.
When imaging the breast using MRI, diffusion-weighted imaging (DWI) aids in diagnosing malignant and benign lesions. Diffusion is affected by tissue properties and obstacles, and it is restricted in tissues with a high cellular density.
"In malignant lesions, the cells are more densely packed and the extracellular space is reduced, in comparison with benign lesions and normal breast tissue," Wielema and colleagues wrote in their study abstract. "Therefore, diffusion is restricted in malignant lesions."
However, the method of ROI delineation may influence ADC values and lead to different outcomes affecting the differentiation between malignant and benign breast lesions. Most DWI studies use circular, ellipsoidal, or freeform ROIs to enclose as much of the lesion as possible while staying within the hyperintense lesion on diffusion-weighted images. Alternatively, the brightest part of the lesion on the image is captured in the ROI, the hypointense part at the ADC map, or inside the solid portion of the lesion.
The chosen ROIs
The retrospective study included 41 consecutive women (ages 22-75, mean age 47) with 50 mass-enhanced breast lesions (44 malignant, six benign), having an area of 0.8 cm2 or greater. The average lesion was 2.0 cm2.
The researchers acquired all MR images on a 1.5-tesla system (Magnetom Avanto, Siemens Healthineers) with patients in the prone position. The MRI protocol consisted of transversal dynamic contrast-enhanced (DCE) T1-weighted, diffusion-weighted images with b-values of 0, 50, 200, 500, 800, and 1,000 s/mm2. Precontrast ADC maps were automatically calculated from the b = 0 and b = 1,000 s/mm2 DWI series by dedicated software.
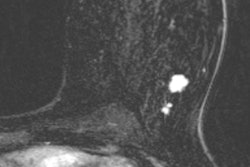
Three observers independently drew four types of ROIs. Observer 1 chose the largest cross-section MRI slice, based on the lesion diameter on DCE-T1. All observers placed ROI1 as an oval shape on that same slice, to encompass most of the lesion, while staying within its borders on the subtracted DCE-T1 series, and copied ROI1 to the diffusion-weighted images with b-values of 0 and 1,000 s/mm2. ROIs 2, 3, and 4 with standard size and shape were positioned on b-values 0 and 1,000 s/mm2 as well.
ROI2 was a standardized circle of 0.3 cm2 positioned in the middle of the lesion. ROI3 and ROI4 also were circular with fixed areas of 0.3 cm2 and 0.6 cm2, respectively, and positioned inside ROI1 so the lowest mean ADC was obtained, the researchers noted.
Of the 50 breast lesions, 44 (88%) were malignant. The malignant breast lesions were invasive ductal carcinoma (41) or invasive lobular carcinoma (three). The size of ROI1 for malignant lesions varied between 0.8 cm2 and 8.4 cm2. For the six benign lesions (12%), the size varied between 0.8 cm2 and 6.3 cm2.
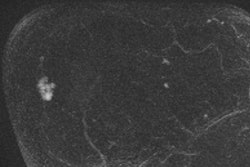
Significant differences in ADC values of benign and malignant breast lesions were not observed in the entire lesion (ROI1) or in its center (ROI2), but they did apply to the minimum ADC subregions of fixed size and shape: ROI3 (p = 0.008) and ROI4 (p = 0.044), according to the researchers.
Receiver operating characteristic (ROC) analysis showed the highest area under the curve (AUC) for ROI3, 0.706, which was consistent with the differentiation between benign and malignant lesions obtained with the small ROI minimum ADC fixed circle method (p = 0.008).
"Any of the alternative ROI methods, featuring either fixed-size ROIs in the middle of the lesion (ROI2, 0.3 cm2), or ones at lowest ADC (ROI3, 0.3 cm2; ROI 4, 0.6 cm2), yielded strong inter- and intraobserver agreements, similar to those of ROI1," Wielema and colleagues noted.
However, the results are preliminary and must be validated with more breast lesions and in a prospective study before they can be incorporated into clinical practice, they concluded.