Breast MRI pioneer Dr. Christiane Kuhl has demonstrated that an abbreviated scanning protocol of just three minutes could make breast MRI a reality for population-based screening. The protocol worked well in a research study of more than 400 women that was published in the August issue of the Journal of Clinical Oncology.
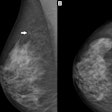
Breast MRI is known to be highly sensitive for detecting breast cancer, but the modality is time-consuming, taking up to 40 minutes to acquire a single study. Contrast that with the high-throughput environment of screening mammography, where breast radiologists can read up to 100 studies an hour.
As a result, breast MRI has been limited to use as a second-line imaging method to solve diagnostic problems in patients with equivocal findings on mammography or ultrasound.
"In these women, MRI screening shifts the stage distribution of breast cancers toward lower stages and reduces the fraction of interval cancers," wrote Kuhl, from the diagnostic and interventional radiology department at the University of Aachen in Germany, and colleagues (J Clin Oncol, August 2014, Vol. 32:22, pp. 2304-2310). "Although results from randomized prospective screening trials are lacking, there is indirect evidence to suggest that MRI screening helps improve the prognosis of women at increased risk of breast cancer."
If MRI is to be used to screening purposes, it must mirror mammography screening in that it becomes standardized and relatively simple. Thus, the researchers sought to determine whether an abbreviated MRI protocol is feasible.
Limited MRI protocol
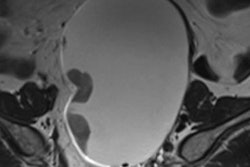
The researchers developed an abbreviated MRI protocol that limited sequences to one pre- and one postcontrast T1-weighted acquisition (GE Healthcare) that takes approximately 120 seconds for image acquisition, plus the time needed for placing the patient on the table, starting the IV line, and injecting the contrast agent.
They also used standard image reconstruction tools to allow a fast overview of the imaging volume, with expert radiologists interpreting the limited protocol.
The prospective observational reader study included 443 women who were mildly to moderately at risk of breast cancer, with 606 screening MRI exams conducted. Eligible women had normal or benign digital mammograms and, for those with heterogeneously dense or extremely dense breasts, normal or benign ultrasounds studies.
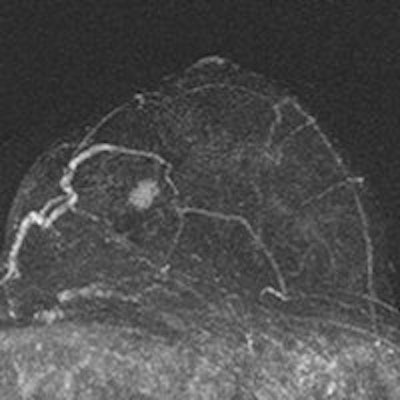
Radiologists reviewed maximum intensity projection (MIP) images first to look for significant enhancement, and then reviewed the complete abbreviated protocol consisting of MIP and first postcontrast subtracted fast images (and optionally nonsubtracted source images) to determine a diagnosis. Only after that was the regular full diagnostic protocol analyzed.

The MRI acquisition time for the full diagnostic protocol was 17 minutes, compared with three minutes for the abbreviated protocol. Average time to read the single MIP was 2.8 seconds, compared with 28 seconds to review the entire abbreviated protocol. The readers detected 11 breast cancers (four ductal carcinomas in situ and seven invasive cancers; all T1N0 intermediate or high-grade), for an additional cancer yield of 18.2 per 1,000, the researchers wrote.
MIP readings were positive in 10 (90.9%) of 11 cancers and showed a negative predictive value (NPV) of 99.8% (418 of 419). Readers using the complete abbreviated protocol diagnosed all 11 cancers. Specificity and positive predictive value (PPV) of the abbreviated protocol versus the full diagnostic protocol were equivalent (94.3% versus 93.9% and 24.4% versus 23.4%, respectively).
Population-based screening MRI
The study indicates that breast MRI could be ready for widespread use on a population basis, Kuhl reported.
"Our aim was to show that true screening MRI, i.e., abbreviated MRI, is indeed a method that can be used for population-based mass screening, because it provides everything a screening examination should offer: very high sensitivity, a high specificity/PPV, short acquisition times, no radiation, and, almost most importantly: very short reading times," Kuhl wrote in an email to AuntMinnieEurope.com.
She pointed out that the reading time for a MIP (less than 3 seconds) is faster than for a mammogram and much faster than the time required to complete a screening ultrasound.
But she offered one important caveat: Expert radiologists must interpret the images to make it effective. This is in accordance with screening mammography, where experts interpret mammograms -- in the European Union, screening radiologists need to review 5,000 cases (20,000 mammograms) per year to maintain their license, according to Kuhl.
"You certainly do not need 5,000 MRI studies, but our experts had at least three years' experience in interpreting a case load of about 500 breast MRIs per year," she wrote. "This approach cannot be transferred into every community radiology setting, but requires specific expertise. However, just as with screening mammography, this expertise will develop with demand. The same issue existed before the advent of screening mammography."
In terms of what's next, Kuhl and colleagues are about to publish their results on using MRI to screen women with an average risk of breast cancer. She also said together with Dr. Chris Comstock from Memorial Sloan Kettering Cancer Center in New York City and Dr. Gillian Newstead from the University of Chicago in Illinois, U.S., she is trying to initiate an Eastern Cooperative Oncology Group (ECOG) and American College of Radiology Imaging Network (ACRIN) trial on using the abbreviated protocol in women with average risk and compare it with digital breast tomosynthesis.