Clinical 7-tesla MRI is no longer a distant pipedream for researchers and is gaining ground in routine scenarios, advocates of the technique state. Its growing pertinence for diseases such as multiple sclerosis, epilepsy, and dementia means that radiologists need to know about the latest 7-tesla practice and its potential, but some practical issues still remain.
The possibility of 7-tesla revealing increased anatomical detail and achieving better contrast-to-noise ratio (CNR) of brain structures and brain pathology can help to increase the confidence in several diagnoses, including microinfarcts, pituitary microadenomas, and cortical dysplasia in epilepsy patients, according to the technique's supporters.
"At the end of the day, the CNR of 7-tesla is more important than the increased signal-to-noise ratio (SNR), compared to 3-tesla and 1.5-tesla MRI. This means that 7-tesla can better detect pathologies, including small lesions," noted Dr. Jeroen Hendrikse, chair of the radiology department at the University Medical Center (UMC) in Utrecht, the Netherlands. "Furthermore, methods to improve CNR at 7-tesla can also be exploited for better diagnosis at 3 tesla and 1.5 tesla, as has been shown for the detection of cortical microinfarcts."
Specifically, he discussed at ECR 2019 how recent work shows that 7-tesla detects small pituitary adenomas in patients with Cushing's syndrome when no pituitary lesion was detected at lower MRI field strengths. Furthermore, 7-tesla vessel wall imaging can depict the burden of intracranial atherosclerosis, including small intracranial plaques. However, he sounded a note of caution.
"Detailed imaging at 7-tesla will result in the visibility of more vascular and parenchymal lesions and care should be taken to use the modality for diagnostic imaging only in patients with a high risk of disease to avoid false positive diagnosis," Hendrikse told ECR Today ahead of the congress.
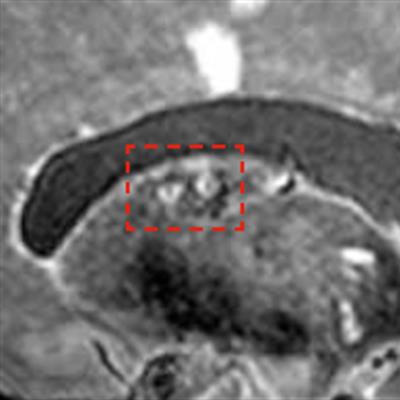
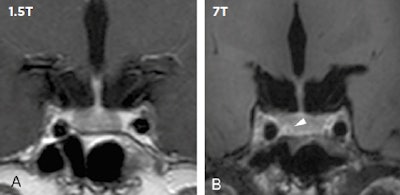 In clinical imaging, 7-tesla MRI can make a difference in detecting and ruling out pituitary lesions. Compared with low-field MRI, 7-tesla MRI in 16 patients resulted in three newly detected pituitary lesions (shown by the white arrow), which had direct implications for neurosurgical planning (see de Rotte, Groenewegen A, Rutgers DR et al, European Radiology, January 2016, Vol. 26:1, pp. 271-277). All images courtesy of Dr. Jeroen Hendrikse.
In clinical imaging, 7-tesla MRI can make a difference in detecting and ruling out pituitary lesions. Compared with low-field MRI, 7-tesla MRI in 16 patients resulted in three newly detected pituitary lesions (shown by the white arrow), which had direct implications for neurosurgical planning (see de Rotte, Groenewegen A, Rutgers DR et al, European Radiology, January 2016, Vol. 26:1, pp. 271-277). All images courtesy of Dr. Jeroen Hendrikse.Nevertheless, it's an exciting time for 7-tesla application, with potential for its use in the assessment of the total burden of disease and in clinical neurodegenerative disease research, allowing the quantification of flow in the small perforating arteries, which is crucial in the development of small vessel disease, such as white-matter lesions of presumed vascular origin.
"In clinical research, 7-tesla not only allows these perforating arteries to become visible with detailed time-of-flight MR angiography (MRA) methods but also quantifies the flow velocity profiles of these perforating arteries in the deep gray matter and the deep white matter with phase-contrast MRA methods. Until now only the parenchyma correlates, or white-matter lesions, could be seen with MRI; the underlying vascular disease was presumed, but could not be quantified or investigated," he noted.
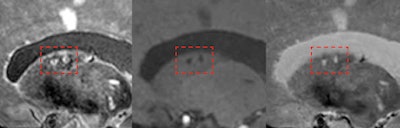 7-tesla MRI can detect the total burden of larger and smaller infarcts, including small microinfarcts in the deep gray matter (shown here inside red frames).
7-tesla MRI can detect the total burden of larger and smaller infarcts, including small microinfarcts in the deep gray matter (shown here inside red frames).So just how soon will 7-tesla be seen in the routine clinical arena? The jury is still out, but it may be coming fairly soon, according to Hendrikse. In fact, it already is here for specific indications, particularly patients with a high prior risk of a pituitary adenoma with undetected lesions at lower MRI field strengths and patients for whom an important clinical decision has to be made, such as for neurosurgery, he added.
Aiming to enlighten ECR delegates about the power and plurality of 7-tesla for cardiovascular and abdominal imaging during today's session, Dr. Jeanette Schulz-Menger, director of the Cardiovascular MR Working Group at Charité University Hospital in Berlin, highlighted 7-tesla MRI's potential as a multidisciplinary modality.
"I hope to convince radiologists at the session that clinical 7-tesla is not crazy or undoable, but also that it is not always the solution," she told ECR Today.
At the Erwin L. Hahn Institute for Magnetic Resonance Imaging in Essen, 7-tesla MRI is already guiding therapeutic decision-making ahead of brain surgery for differentiation of dissection, plaque formation, and stenosis, she said.
Translating the power of 7-tesla to cardiology brings hitherto unseen benefits, according to cardiologist Schulz-Menger: 7-tesla can identify small structures, potentially highlighting which patients will go into heart failure, and while it is not ready for deployment tomorrow, nor is this application too far off.
Clinicians need to be aware of 7-tesla's dual capacity to show tissue contrast and movement, she noted. Furthermore, in the abdomen, 7-tesla can detect renal artery stenosis without the need for contrast agents, which has advantages for patients. Despite the challenges of abdominal imaging, 7-tesla offers a means to quantify pathophysiology, detect perfusion, and potentially measure deoxygenation of the kidneys.
"Without doubt, 7-tesla is a motor that is enhancing understanding, guiding therapy decisions, and creating new possibilities for depicting static anatomy and pathophysiology without the use of contrast. The question is: Do radiologists want to follow it or drive it?" she noted.
While work across the 7-tesla cardiac community used to be focused on developing a stable gating device to reduce 7-tesla "black holes" and motion artifacts, now the biggest challenge is the capacity to generate fast homogeneous images regardless of different coil structures, Schulz-Menger said. She also stressed that deployment of 7-tesla in clinical routine must be vendor-driven, and for that there needs to be approval by the regulatory authorities.
Several centers are already using 7-tesla for imaging multiple sclerosis. In Berlin, group collaborations are also working on how to deploy 7-tesla to measure sodium and potassium in the heart as a means to explain arterial hypertension, using dedicated coils for quantification, while others are exploring noninvasive hemodynamics. With such clinical information, doctors can edge nearer to providing personalized medicine to their patients, according to Schulz-Menger.
She added that it is important for radiologists and cardiologists to work together with other users of 7-tesla to reduce turf friction and put patients first.
"I personally train both radiologists and cardiologists in [cardiac MR]. Those who do it best should take it forward," she concluded.
Originally published in ECR Today on 28 February 2019.
Copyright © 2019 European Society of Radiology



















